WFUMB Position Statement: How to perform a safe ultrasound examination and clean equipment in the context of COVID-19
March 27, 2020AAA Quiz
April 7, 2020Due to the still growing pandemia of SARS-COV-2 we have decided to show a case from a patient suffering from COVID-19 pneumonia. We thank our Italian colleagues for providing the case illustrating the different lung ultrasound findings. We thank you for your support even in these difficult times.
Our thoughts are with you.
Kind regards
Tobias and Caroline (WFUMB Case of the Month Editors)
Ultrasound findings in COVID-19 pneumonia
Authors and affiliations
Dr. Soccorsa Sofia, Dr. Michele Spampinato
Emergency Department, Local Health Unit, Bologna, Italy
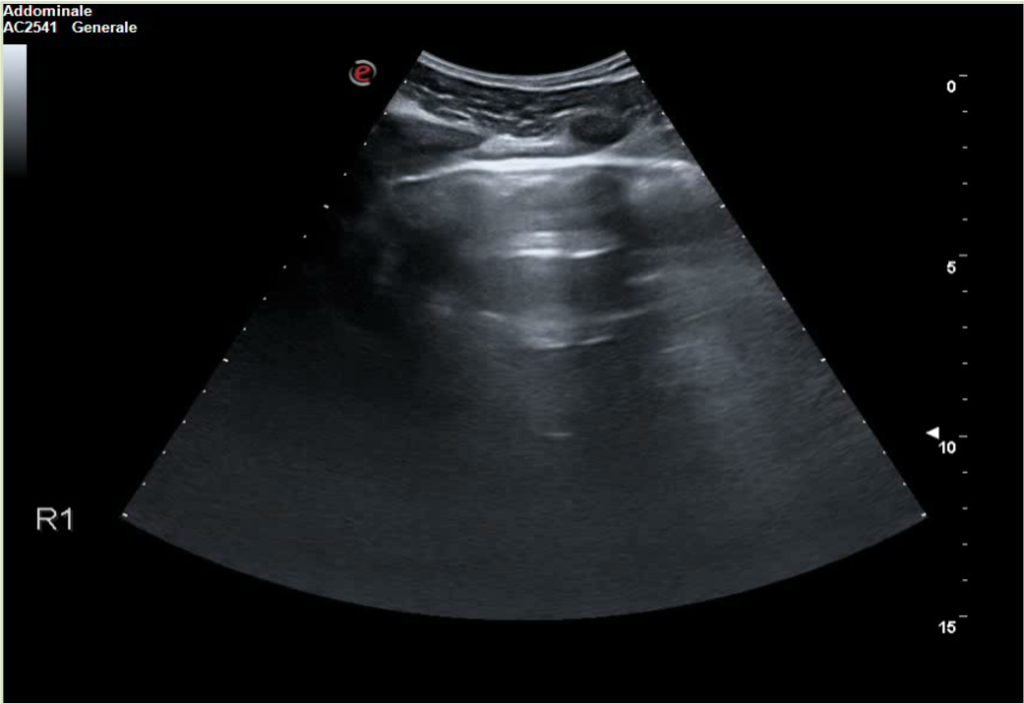
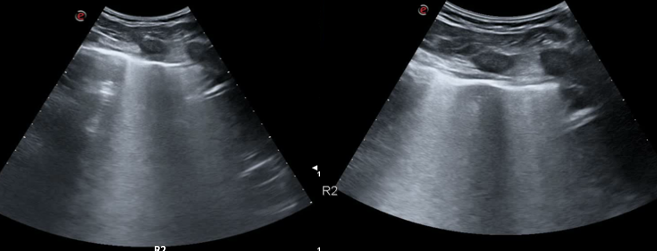
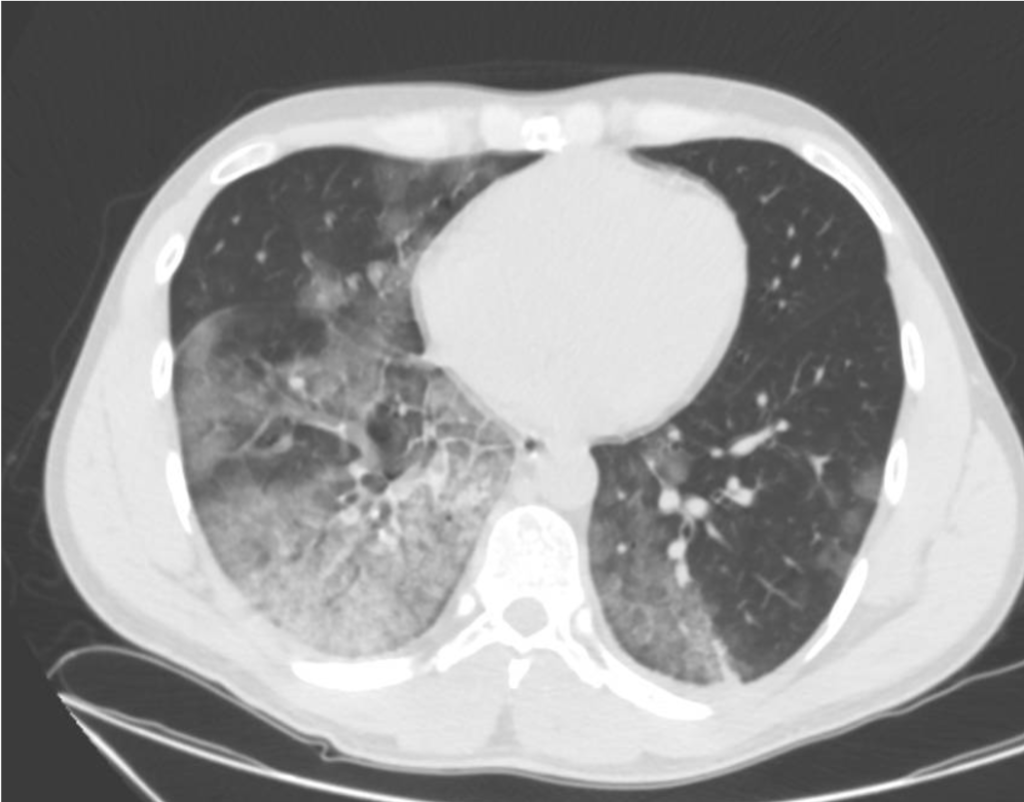
Clinical history
A 30-year-old man presents to the emergency department (ED) due to syncope. For the last 10 days he had had fever, cough and dyspnea. At the ED his peripheral oxygen saturation was 86%, BP 130/80, HR 88bpm, RR 20 /min and his temperature 37.4°C. He was given oxygen on a mask. Chest CT was performed and later lung ultrasound (LUS) was performed in 12 areas longitudinal/oblique views using a convex array probe followed by a linear array probe for details (figure 1).
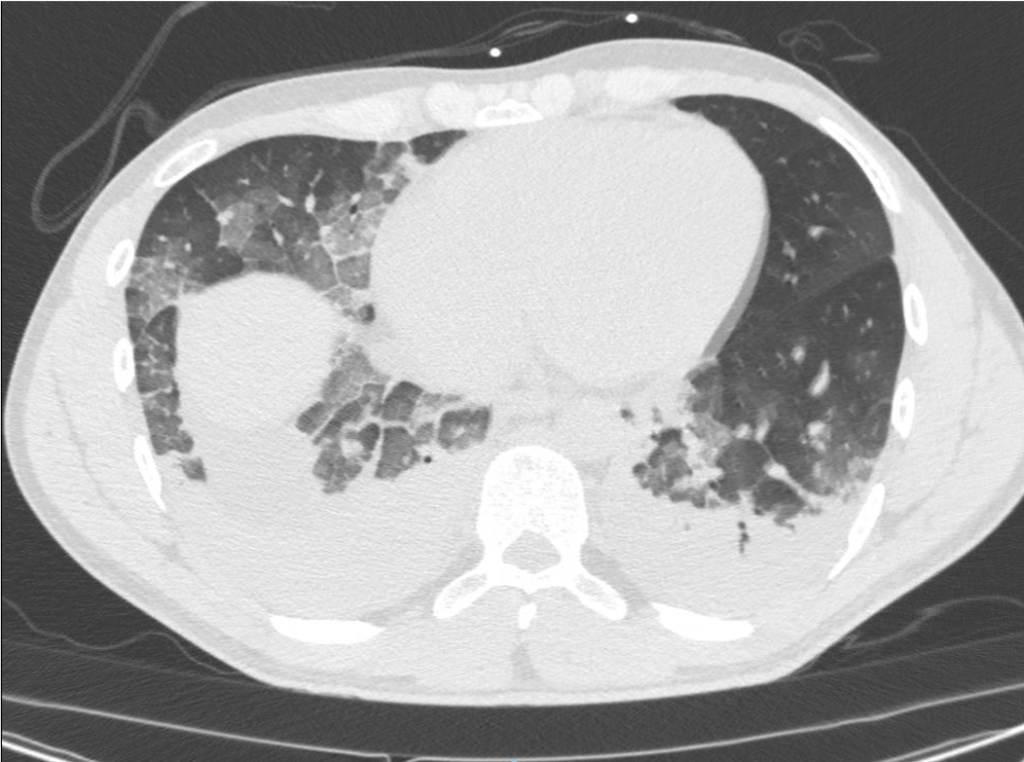
The patient was tested positive for SARS-COV-2. On day 2 after admission the patient’s condition deteriorated, and he was transferred to the ICU. Another chest CT was performed. We show the ultrasound and CT images with corresponding legends (image 1-7 + video 1) and discuss the findings in relation to the diagnostic work-up of COVID-19 pneumonia.
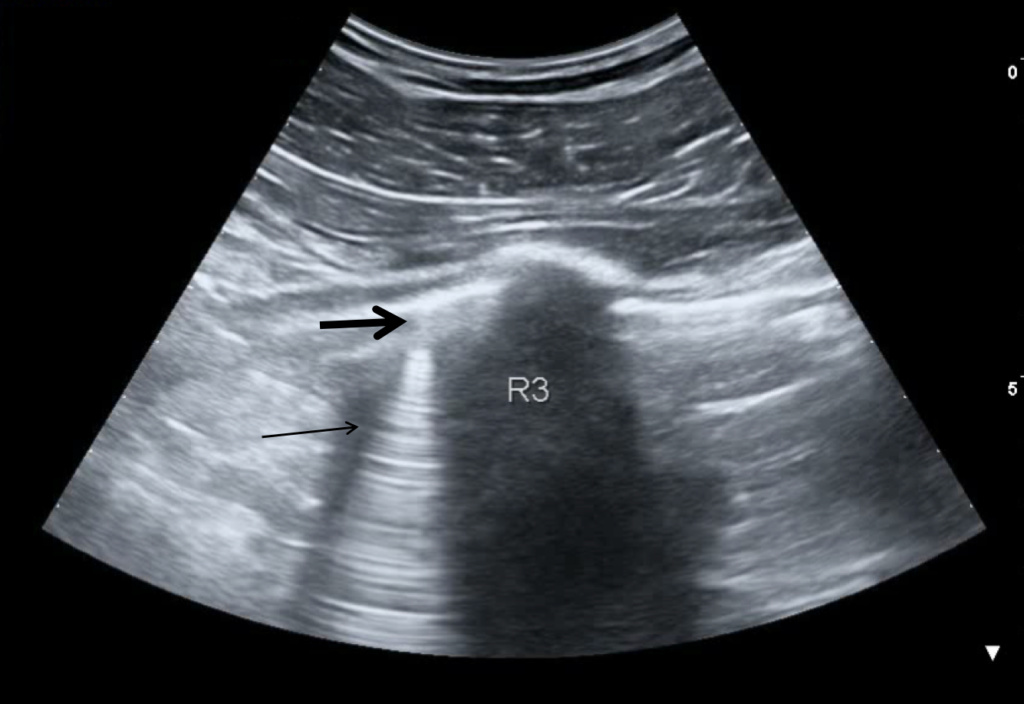
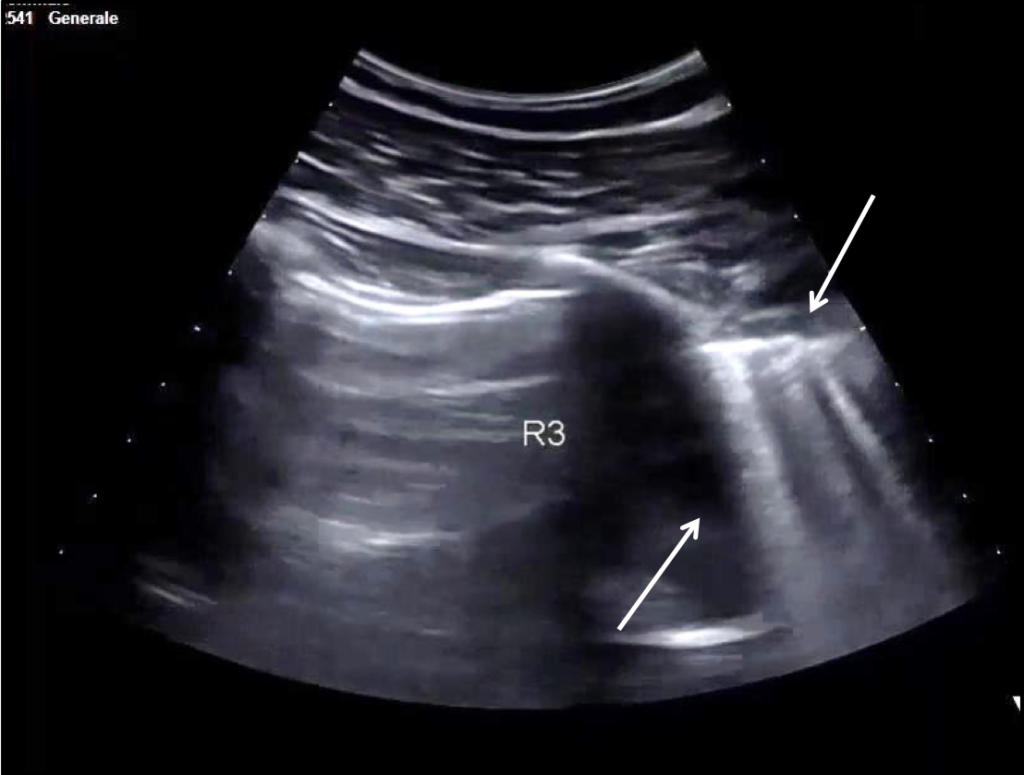

Video 1: Lung consolidation in the basal segment of the lower right lobe after patient deterioration (day 2).
Discussion
Most patients with COV2 related disease present with fever, cough, muscle pain, chest discomfort and later dyspnea. More rarely sore throat and intestinal symptoms may be present. 81% of infections are mild (flu-like symptoms); 13.8% of patients develop severe disease including pneumonia and shortness of breath, usually about one week after symptom onset; 4.7% are critical and suffer from respiratory failure, septic shock and multiorgan failure; and in 2.5-7.8% of cases (depending on country and available data) the infection is fatal. The risk of death increases in older patients.
On imaging initial lesions are usually peripheral because SARS-COV-2 attacks the small distal airways. Several reports have described the findings in chest CT. Most commonly few, small, segmental ground glass opacities are seen peripherally and basal. These may deteriorate to become bilateral and multisegmental and finally consolidation and/or ARDS.
Most common LUS signs are: vertical pleurogenic artifacts with varying degree of intensity (from few to confluent). These alternate with clear demarcation to A-lines in the same area, especially in the mid- and upper lung. Pleural thickening, sometimes marked, due to the presence of numerous, small subpleural consolidations. Lobar or translobar consolidations of large size and minimal pleural effusions. The LUS features match with the site and kind on CT.
LUS is an examination, which can be carried out bedside. It may provide early information of presence of diffuse multifocal pneumonia (as in COVID-19) and its deterioration (enlarging consolidations). By doing LUS in cases with COVID-19 pneumonia, transport of patients through the hospital and unnecessary exposure of staff and other patients is avoided.
Similar LUS signs as the ones described have been observed in other kinds of viral epidemic pneumonia. If they, individually or in combination, have some specificity for COVID-19 pneumonia it should be established with further appropriate studies.
References
- Tsung JW et at. Prospective application of clinician-performed lung ultrasonography during the 2009 H1N1 influenza A pandemic: distinguishing viral from bacterial pneumonia. Critical Ultrasound Journal (2012) 4:16
http://www.criticalultrasoundjournal.com/content/4/1/16
- Zhang et al. Lung ultrasonography for the diagnosis of 11 patients with acute respiratory distress syndrome due to bird flu H7N9 infection.Virology Journal (2015) 12:176 DOI 10.1186/s12985-015-0406-1
- Li-Li Ren et al. Identification of a novel coronavirus causing severe pneumonia in human: a descriptive study Chinese Medical Journal (2020) Vol(No) www.cmj.org
- 4. Huang C et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet (2020) Jan 24 [Epub ahead of print].
- Chung M et al. CT Imaging Features of 2019 Novel Coronavirus (2019-nCoV). Radiology 2020; xxx:xxx–xxx https://doi.org/10.1148/radiol.2020200230
- Bernheim Adam et al. Chest CT Findings in Coronavirus Disease-19 (COVID-19): Relationship to Duration of Infection Radiology Feb 20 2020 https://doi.org/10.1148/radiol.2020200463
- Qian‐Yi Pengand Chinese Critical Care Ultrasound Study Group (CCUSG) Findings of lung ultrasonography of novel corona virus pneumonia during the 2019-2020 epidemic . Intensive Care Med https://doi.org/10.1007/s00134-020-05996-6