WFUMB / EFSUMB Students Webinar Series: 26 November 2022
November 28, 2022
WFUMB Webinar: Hand Held Ultrasound Devices 19-01-2023
December 15, 2022Chenxi Huang 1,*, Bo Nyhuus 2
1 Department of Radiology, Copenhagen University Hospital, Rigshospitalet, Copenhagen, Denmark; chenxihuang@msn.com
2 Department of Radiology, Copenhagen University Hospital, Rigshospitalet, Copenhagen, Denmark;
* Correspondence: chenxihuang@msn.com
Clinical history
A 60-year-old male, who had previously undergone Whipple’s procedure due to biliary IPMN was listed for liver transplantation. The first transplantation failed due to biliary tree ischemia and cholascos. The second transplantation was complicated by leakage from the Roux limb of the previous hepaticojejunostomy that lead to further surgery. Three days after the most recent surgery (9 days after the 2nd transplantation), the patient developed acute abdominal pain and an increase in serum bilirubin (84; ref 5 – 25 µmol/L), ALAT (256; ref 10 – 70 U/L) and CRP (90; ref < 8 mg/L). A CT of the abdomen without intravenous contrast agent was performed to check for free intraabdominal air, as the patient had previously had an anaphylactic reaction with angioedema due to CT contrast agent.
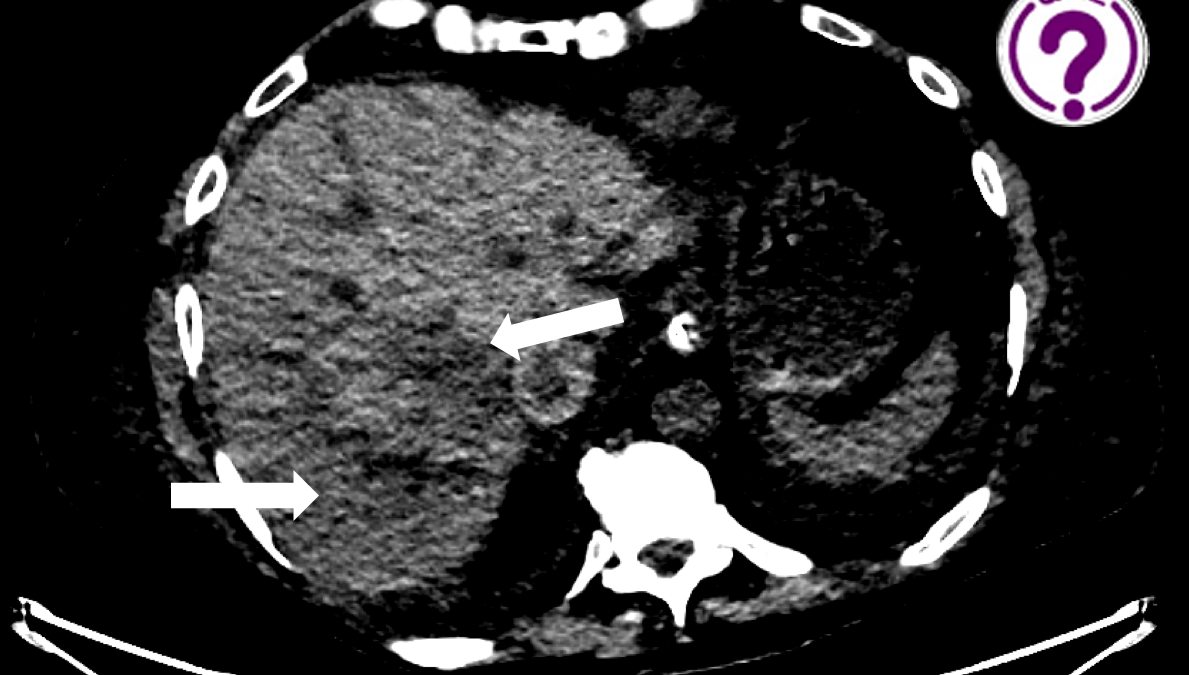
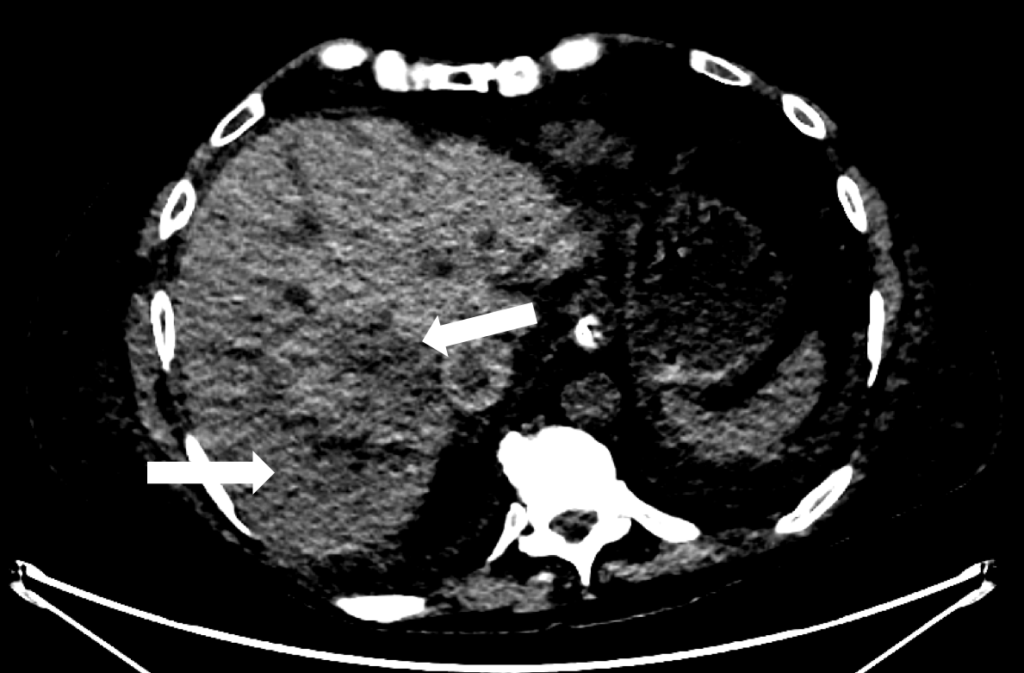
CT of the abdomen without intravenous contrast agent (axial reconstruction, modified soft tissue window)
Quiz-summary
0 of 3 questions completed
Questions:
- 1
- 2
- 3
Information
View the December Case below, answer the question and then click check >
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading...
You must sign in or sign up to start the quiz.
You have to finish following quiz, to start this quiz:
Results
0 of 3 questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 points, (0)
Categories
- Not categorized 0%
- 1
- 2
- 3
- Answered
- Review
-
Question 1 of 3
1. Question
Question 1: What is seen in the liver parenchyma on the CT scan, and what could it represent?
Correct
CORRECT ANSWER EXPLAINED BELOW Correct answer to Q1 is: Inhomogeneity in CT attenuation in the right liver lobe due to infarction or thrombosis or hematoma
The CT scan showed no free air or leakage, but inhomogeneity in CT attenuation in the right liver lobe. Most likely representing infarction, thrombus or hematoma. Therefore, the patient was further examined with abdominal ultrasound to evaluate the vessels.
Incorrect
CORRECT ANSWER EXPLAINED BELOW Correct answer to Q1 is: Inhomogeneity in CT attenuation in the right liver lobe due to infarction or thrombosis or hematoma
The CT scan showed no free air or leakage, but inhomogeneity in CT attenuation in the right liver lobe. Most likely representing infarction, thrombus or hematoma. Therefore, the patient was further examined with abdominal ultrasound to evaluate the vessels.
-
Question 2 of 3
2. Question
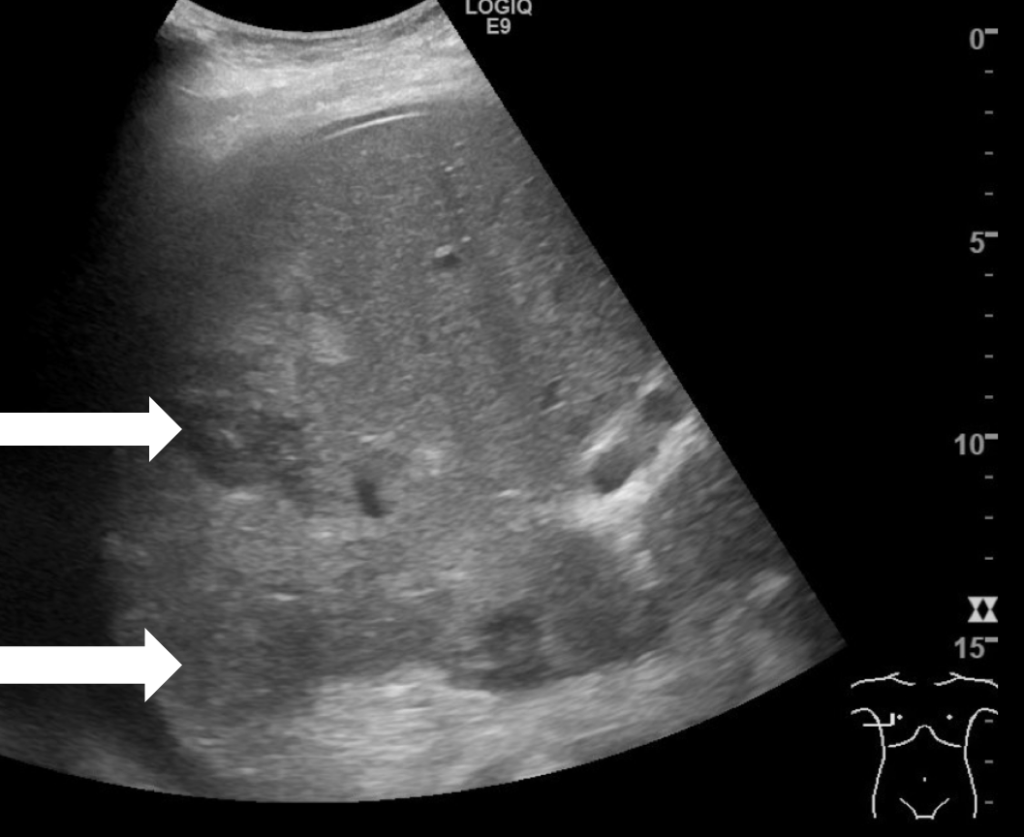
B-mode ultrasound of the right liver lobe, axial plane
Question 2: What does the ultrasound image reveal?
Correct
CORRECT ANSWER EXPLAINED BELOW Correct answer to Q2 is: Focal infarction or thrombosis in the right hepatic vein
There is a long hypoechoic area in segments 7/8 compared to the rest of the liver parenchyma. On colour Doppler no signal was obtained from the right liver vein. The hypoechoic area most likely represents an infarction due to acute thrombosis. It is less likely to be a hematoma, as postoperative hematomas are usually located at the surface or just below the liver capsule. Focal fatty sparing is often located adjacent to the gallbladder. Lastly biloma appears like a cyst, which is anechoic, has posterior acoustic enhancement and often a round shape.
Incorrect
CORRECT ANSWER EXPLAINED BELOW Correct answer to Q2 is: Focal infarction or thrombosis in the right hepatic vein
There is a long hypoechoic area in segments 7/8 compared to the rest of the liver parenchyma. On colour Doppler no signal was obtained from the right liver vein. The hypoechoic area most likely represents an infarction due to acute thrombosis. It is less likely to be a hematoma, as postoperative hematomas are usually located at the surface or just below the liver capsule. Focal fatty sparing is often located adjacent to the gallbladder. Lastly biloma appears like a cyst, which is anechoic, has posterior acoustic enhancement and often a round shape.
-
Question 3 of 3
3. Question
To further visualize the vessels a contrast enhanced ultrasound examination (CEUS) was performed by a senior consultant the next morning.
CEUS of the liver in arterial, early venous and late venous phases, respectively.
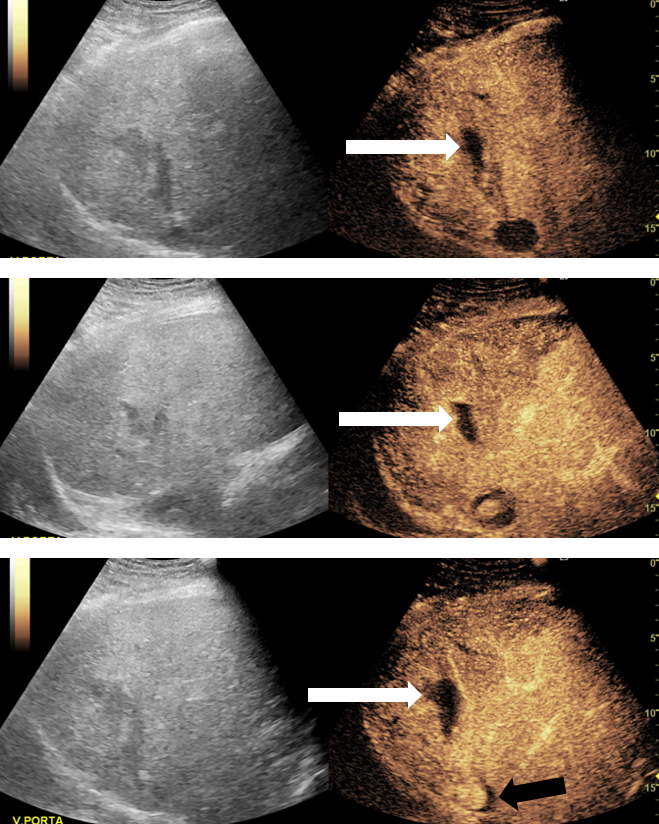
Image 3, 4, 5 and video 1. CEUS demonstrates a persisting filling defect during the entire examination. They correspond to the hypoechoic area(s) in B-mode, marked by the white arrow. In addition there was a half-moon sharped filling defect in the IVC in the late venous phase, marked by the black arrow in image 5.
Question 2: What is the most likely diagnosis due to the current ultrasound findings?
Correct
CORRECT ANSWER EXPLAINED BELOW Correct answer to Q3 is: Focal liver infarction and mural thrombosis in the IVC
Discussion:
The contrast enhanced ultrasound images (CEUS) revealed a focal infarction (contrast defect) in the liver and a mural thrombosis in the IVC and the right liver vein. The mural thrombosis becomes apparent as a filling defect in the IVC, which remained in the late phase.
Ultrasound is a very important tool in evaluating the liver for post-transplantation complications. Many complications can occur soon after transplantation, incl. vascular, biliary and infectious complications. Hepatic artery thrombosis is the most significant complication and is often associated with graft failure (1). If the graft survives, biliary ischemia may, in turn, lead to a non-anastomotic biliary stricture or leak resulting in a biloma. Thrombosis can also occur in other vessels such as the portal and hepatic veins leading to partial infarction. In addition, most patients are treated with immunosuppressive drugs that make the graft prone to infections and abscess. Finally, bleeding and leakage from the anastomoses are also serious complications (1).
Ultrasound provides a tool to evaluate the liver parenchyma, biliary tree, and vessels for abnormalities. Colour and Spectral Doppler enable us to check the blood supplies to the liver graft by measuring RI-indices and vascular acceleration, without any radiation and exposure to CT contrast agents (2). Furthermore, it may be performed in the intensive care unit.
CEUS becomes a very important tool, in cases like ours, where the patient does not tolerate CT contrast agent. With CEUS, we can evaluate the enhancement of the liver parenchyma, the vessel patency and the complications of the graft, including arterial and venous stenosis, infarction and necrosis, abscess, hematomas, and malignancy (2).
In conclusion, ultrasound and CEUS are important tools in evaluating post-transplantation complications including vascular and infectious complications.
Conflicts of interest
“The authors declare no conflict of interest.”
References
- Singh AK, Nachiappan AC. Postoperative imaging in liver transplantation: what radiologists should know. Radiographics. 2010 Mar;30(2):339-51.
- Girometti R, Como G, Bazzocchi M, Zuiani C. Post-operative imaging in liver transplantation: state-of-the-art and future perspectives. World J Gastroenterol. 2014 May 28;20(20):6180-200
Incorrect
CORRECT ANSWER EXPLAINED BELOW Correct answer to Q3 is: Focal liver infarction and mural thrombosis in the IVC
Discussion:
The contrast enhanced ultrasound images (CEUS) revealed a focal infarction (contrast defect) in the liver and a mural thrombosis in the IVC and the right liver vein. The mural thrombosis becomes apparent as a filling defect in the IVC, which remained in the late phase.
Ultrasound is a very important tool in evaluating the liver for post-transplantation complications. Many complications can occur soon after transplantation, incl. vascular, biliary and infectious complications. Hepatic artery thrombosis is the most significant complication and is often associated with graft failure (1). If the graft survives, biliary ischemia may, in turn, lead to a non-anastomotic biliary stricture or leak resulting in a biloma. Thrombosis can also occur in other vessels such as the portal and hepatic veins leading to partial infarction. In addition, most patients are treated with immunosuppressive drugs that make the graft prone to infections and abscess. Finally, bleeding and leakage from the anastomoses are also serious complications (1).
Ultrasound provides a tool to evaluate the liver parenchyma, biliary tree, and vessels for abnormalities. Colour and Spectral Doppler enable us to check the blood supplies to the liver graft by measuring RI-indices and vascular acceleration, without any radiation and exposure to CT contrast agents (2). Furthermore, it may be performed in the intensive care unit.
CEUS becomes a very important tool, in cases like ours, where the patient does not tolerate CT contrast agent. With CEUS, we can evaluate the enhancement of the liver parenchyma, the vessel patency and the complications of the graft, including arterial and venous stenosis, infarction and necrosis, abscess, hematomas, and malignancy (2).
In conclusion, ultrasound and CEUS are important tools in evaluating post-transplantation complications including vascular and infectious complications.
Conflicts of interest
“The authors declare no conflict of interest.”
References
- Singh AK, Nachiappan AC. Postoperative imaging in liver transplantation: what radiologists should know. Radiographics. 2010 Mar;30(2):339-51.
- Girometti R, Como G, Bazzocchi M, Zuiani C. Post-operative imaging in liver transplantation: state-of-the-art and future perspectives. World J Gastroenterol. 2014 May 28;20(20):6180-200