Case of the Month August 2023 – Importance of contrast enhanced ultrasound in assessment of the uterus
August 1, 2023
WFUMB AFSUMB Student Webinar on Salivary Gland and Prostate
October 2, 2023Martin Necas 1*, Claire Calver 1 & Nicole Curtis 2
1 Waikato Hospital, Hamilton & University of Auckland, New Zealand
2 University of Otago, Dunedin, New Zealand
* Correspondence: martin@antegrade.net
Clinical history
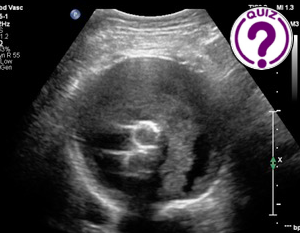
An 83-year-old male received an emergency endovascular aortic repair (EVAR) for a symptomatic (‘pre-rupture’) large (9.0 cm) abdominal aortic aneurysm (AAA). Initial ultrasound (US) one day later reported a small endoleak. Follow-up with US 6 weeks later demonstrated the same appearance.
Images
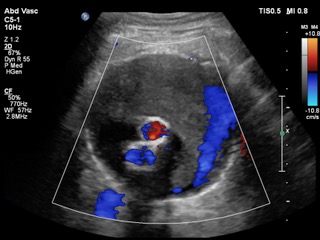
Video 1: Colour Doppler video of the AAA sac.
Quiz-summary
0 of 2 questions completed
Questions:
- 1
- 2
Information
View the May Case below, answer the question and then click check >
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading...
You must sign in or sign up to start the quiz.
You have to finish following quiz, to start this quiz:
Results
0 of 2 questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 points, (0)
Categories
- Not categorized 0%
- 1
- 2
- Answered
- Review
-
Question 1 of 2
1. Question
Question 1: What is your diagnostic impression and what is the next step in the work-up of this patient?
Correct
CORRECT ANSWER EXPLAINED BELOW Correct answer to Q1 is: The finding is suspicious for an endoleak. Further imaging should be performed immediately.
Incorrect
CORRECT ANSWER EXPLAINED BELOW Correct answer to Q1 is: The finding is suspicious for an endoleak. Further imaging should be performed immediately.
-
Question 2 of 2
2. Question
Discussion
B-mode and colour Doppler US are the most common tools for the surveillance of EVAR. The role of B-mode US is to monitor AAA sac size. In this case, the AAA has remained stable which is somewhat reassuring. The role of colour Doppler ultrasound is to detect endoleak(s) by visualising Doppler shifts in the AAA sac. In this case, pulsatile flow is visualised within the AAA suggesting the presence of an endoleak.
It is important to acknowledge that colour Doppler is an imperfect tool for endoleak detection. First, colour Doppler has suboptimal sensitivity to slow endoleaks. Second, colour Doppler is not specific to blood flow. This is because Doppler detects all forms of tissue motion. Under normal circumstances, the assumption that Doppler shifts from rhythmically moving contents within blood vessels represent blood flow is indeed correct. However, in specific circumstances, this assumption is false, which is why CEUS or CTA should be performed.
CEUS is the test of choice at our facility because of its many advantages over contrast CT:
- CEUS can be performed immediately, without delay
- CEUS is the most sensitive test for the detection of endoleaks1,2
- CEUS does not expose the patient to ionising radiation
- CEUS does not require the user to check the patient’s renal function
- CEUS has far lower rate of contrast reactions than CT
- CEUS is significantly cheaper than CT
- CEUS does not place additional resource requirements on the health system because it can be incorporated into the current examination
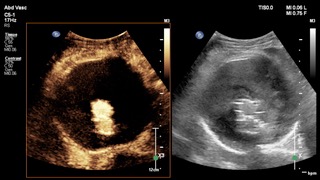
Additional Images
Image 3: CEUS was performed and the AAA sac was observed for several minutes to allow the circulating microspheres to distribute throughout the entire circulatory system. At no phase of CEUS imaging were any microspheres visualised within the AAA sac.
Question 2: What is your final impression?
Correct
CORRECT ANSWER EXPLAINED BELOW Correct answer to Q2 is: No endoleak, but liquefied thrombus circulating within the AAA sac
Additional discussion
CEUS is the most sensitive imaging test for the detection of endoleaks.1,2 CEUS is also easy to implement and perform.3 For these reasons, some centres have incorporated CEUS into their routine EVAR surveillance programmes2,4 including our Vascular Laboratory at Waikato Hospital (Hamilton, New Zealand). CEUS dramatically improves our confidence in the normal functioning of an EVAR. CEUS also plays an important role with diagnostic work-up of complex EVARs affected by endoleaks. The disadvantages of CEUS include: operator dependance, operator experience and the usual limitations in the quality of ultrasound visualisation related to beam attenuation that affects all modes of ultrasound imaging.
In this case, CEUS conclusively excludes an endoleak. The suspicious appearance noted on colour Doppler represents a pseudoendoleak characterised by liquefied intramural thrombus rhythmically circulating within the AAA in response to aortic pulsation. The movement of the liquefied thrombus creates Doppler shifts that are detected and displayed by the ultrasound system. The display is correct and not artifactual. It just does not represent fresh blood arriving from the systemic circulation.3,5,6 The patient received a CTA which confirmed the absence of an endoleak.
Since the introduction of CEUS in EVAR surveillance, we have identified several pseudoendoleaks. It is likely that some endoleaks previously detected by ultrasound and not visible on CTA in fact represent pseudoendoleaks. It’s increasingly becoming clear that using CTA as the gold standard by which to measure the performance of ultrasound is flawed, because a CTA-negative examination with an endoleak detected on CEUS will be falsely classified as a false positive finding for CEUS, whereas it is a true positive and the CTA is falsely negative.
Conclusion
CEUS is an integral part of ultrasound imaging and should be available in all ultrasound imaging departments associated with vascular surgical units. We recommend including CEUS in EVAR surveillance programmes as an excellent initial assessment tool, as well a powerful problem-solving tool.
Conflicts of Interest:
“The authors declare no conflict of interest.”
References
- Chisci E, Harris L, Guidotti A, Pecchioli A, Pigozzi C, Barbanti E, Ercolini L, Michelagnoli S. Endovascular Aortic Repair Follow up Protocol Based on Contrast Enhanced Ultrasound Is Safe and Effective. Eur J Vasc Endovasc Surg. 2018 Jul;56(1):40-47.
- Zarky A, Zywicka E, Santoro G, Jullian L, Joshi M, Dimitri S. Is contrast-enhanced ultrasound (CEUS) superior to computed tomography angiography (CTA) in detection of endoleaks in post-EVAR patients? A systematic review and meta-analysis. J Ultrasound. 2019 Mar;22(1):65-75.
- Necas M, Keating J, Abbott G, Curtis N, Ryke R de, Hill G. How to set-up and perform contrast-enhanced ultrasound. Australas J Ultrasound Med. 2019;22(2):86–95.
- Castagno C, Conti B, Forliti E. A New CTA-Free Approach to Endovascular Aneurysm Repair (EVAR) Follow Up with Contrast Enhanced Ultrasound (CEUS). Eur J Vasc Endovasc Surg. 2019 Dec 1;58(6):e413–4.
- Necas M, Ferrar D. Liquefied Thrombus Mimicking an Endoleak on Duplex Ultrasound: J Vasc Ultrasound [Internet]. 2021 Oct 13 [cited 2021 Oct 14]; Available from: https://journals.sagepub.com/eprint/GP9D3X5EKHR5KHBABEQJ/full
- Lisik JP, Curry G, Buckenham T. Pseudoendoleak: A post-endovascular aortic repair ultrasound surveillance pitfall – Single institution case series. J Med Imaging Radiat Oncol. 2022 Dec;66(8):1059–64.
Incorrect
CORRECT ANSWER EXPLAINED BELOW Correct answer to Q2 is: No endoleak, but liquefied thrombus circulating within the AAA sac
Additional discussion
CEUS is the most sensitive imaging test for the detection of endoleaks.1,2 CEUS is also easy to implement and perform.3 For these reasons, some centres have incorporated CEUS into their routine EVAR surveillance programmes2,4 including our Vascular Laboratory at Waikato Hospital (Hamilton, New Zealand). CEUS dramatically improves our confidence in the normal functioning of an EVAR. CEUS also plays an important role with diagnostic work-up of complex EVARs affected by endoleaks. The disadvantages of CEUS include: operator dependance, operator experience and the usual limitations in the quality of ultrasound visualisation related to beam attenuation that affects all modes of ultrasound imaging.
In this case, CEUS conclusively excludes an endoleak. The suspicious appearance noted on colour Doppler represents a pseudoendoleak characterised by liquefied intramural thrombus rhythmically circulating within the AAA in response to aortic pulsation. The movement of the liquefied thrombus creates Doppler shifts that are detected and displayed by the ultrasound system. The display is correct and not artifactual. It just does not represent fresh blood arriving from the systemic circulation.3,5,6 The patient received a CTA which confirmed the absence of an endoleak.
Since the introduction of CEUS in EVAR surveillance, we have identified several pseudoendoleaks. It is likely that some endoleaks previously detected by ultrasound and not visible on CTA in fact represent pseudoendoleaks. It’s increasingly becoming clear that using CTA as the gold standard by which to measure the performance of ultrasound is flawed, because a CTA-negative examination with an endoleak detected on CEUS will be falsely classified as a false positive finding for CEUS, whereas it is a true positive and the CTA is falsely negative.
Conclusion
CEUS is an integral part of ultrasound imaging and should be available in all ultrasound imaging departments associated with vascular surgical units. We recommend including CEUS in EVAR surveillance programmes as an excellent initial assessment tool, as well a powerful problem-solving tool.
Conflicts of Interest:
“The authors declare no conflict of interest.”
References
- Chisci E, Harris L, Guidotti A, Pecchioli A, Pigozzi C, Barbanti E, Ercolini L, Michelagnoli S. Endovascular Aortic Repair Follow up Protocol Based on Contrast Enhanced Ultrasound Is Safe and Effective. Eur J Vasc Endovasc Surg. 2018 Jul;56(1):40-47.
- Zarky A, Zywicka E, Santoro G, Jullian L, Joshi M, Dimitri S. Is contrast-enhanced ultrasound (CEUS) superior to computed tomography angiography (CTA) in detection of endoleaks in post-EVAR patients? A systematic review and meta-analysis. J Ultrasound. 2019 Mar;22(1):65-75.
- Necas M, Keating J, Abbott G, Curtis N, Ryke R de, Hill G. How to set-up and perform contrast-enhanced ultrasound. Australas J Ultrasound Med. 2019;22(2):86–95.
- Castagno C, Conti B, Forliti E. A New CTA-Free Approach to Endovascular Aneurysm Repair (EVAR) Follow Up with Contrast Enhanced Ultrasound (CEUS). Eur J Vasc Endovasc Surg. 2019 Dec 1;58(6):e413–4.
- Necas M, Ferrar D. Liquefied Thrombus Mimicking an Endoleak on Duplex Ultrasound: J Vasc Ultrasound [Internet]. 2021 Oct 13 [cited 2021 Oct 14]; Available from: https://journals.sagepub.com/eprint/GP9D3X5EKHR5KHBABEQJ/full
- Lisik JP, Curry G, Buckenham T. Pseudoendoleak: A post-endovascular aortic repair ultrasound surveillance pitfall – Single institution case series. J Med Imaging Radiat Oncol. 2022 Dec;66(8):1059–64.