Case of the Month October 2023 – A liver lesion in the absence of liver disease – is it always so obvious?

WFUMB AFSUMB Student Webinar on Salivary Gland and Prostate
October 2, 2023
WFUMB AFSUMB Student Webinar on Ultrasound safety, technology and development
October 20, 2023Evelina Atanasova 1, Dimitar Popov 1, Christo Pentchev¹, Maria Petkova¹ and Christian Nolsøe2
1 Clinic of Gastroenterology, University Hospital “St. Ivan Rilski” Sofia, Bulgaria; e-mail: eva_gatanasova@abv.bg
2 Centre for Surgical Ultrasound, Department of Surgery, Zealand University Hospital, Køge, Denmark; cnolsoe@cnolsoe.dk
* Correspondence: eva_gatanasova@abv.bg
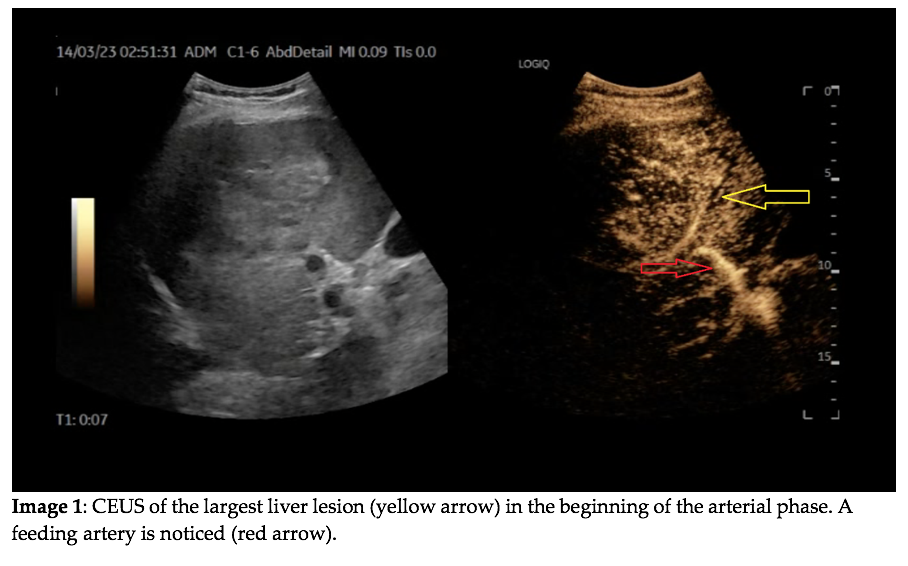
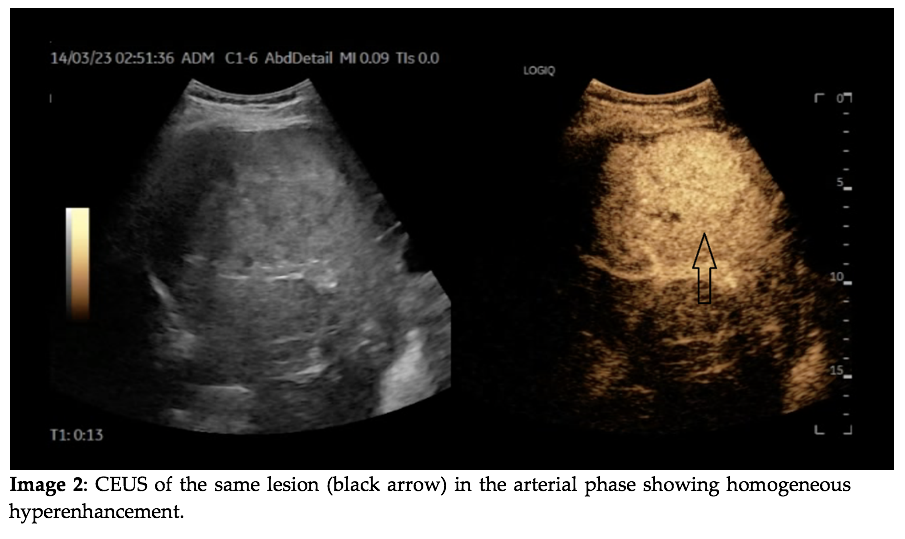
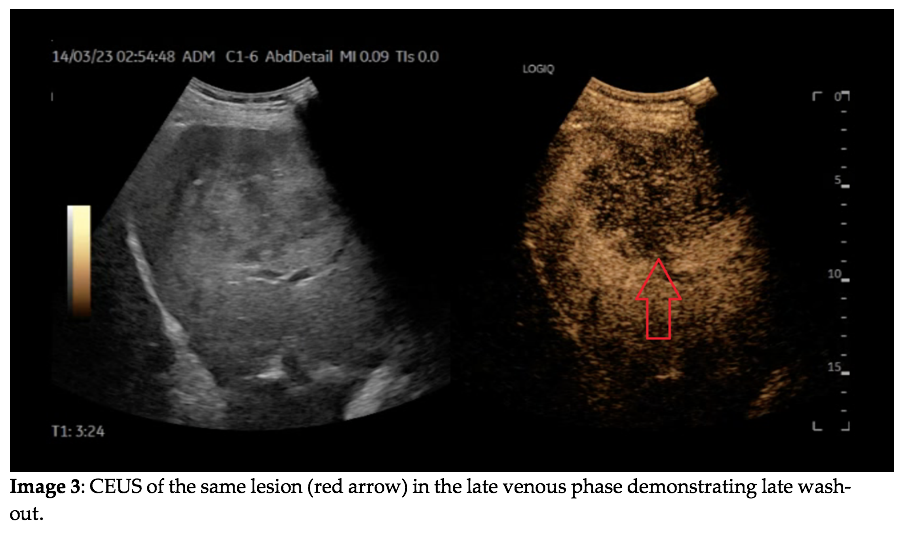
Clinical history
A 59-year-old male patient with a history of an enlarged prostatic gland and no other co-morbidities was admitted to to hospital due to urinary tract obstruction. During the abdominal and pelvic ultrasound scan a large liver lesion was found. The patient was referred to our clinic for further diagnostics.The patient had worked in a metal processing plant and had not had anintake of any toxic substances including excessive alcohol intake. At the admission he had unremarkable blood tests except for slightly elevated cholestatic liver enzymes. Hepatotropic viruses were excluded. The abdominal ultrasound including CEUS described a heterogeneous rounded lesion in the right liver lobe measuring 9.5 cm/7.3 cm, on the periphery of which small arteries were detected. Two smaller lesions measuring 3.8 cm and 1.9 cm were described. For clarification, an upper and lower endoscopy including ileoscopy was performed without any evidence of malignancy. Contrast-enhanced-CT (CE-CT) of the thorax and abdomen (arterial and venous phase for the abdomen) revealed an intensive contrast uptake in the arterial phase of the largest lesions in liver segments VI and VII with central necrotic areas in it, and wash out in the venous phase. Additionally, bone metastases were detected.
Images
Video 1: CEUS of the liver lesion in the arterial phase.
Video 2: CEUS of the liver lesion in the late venous phase.
Quiz-summary
0 of 2 questions completed
Questions:
- 1
- 2
Information
View the May Case below, answer the question and then click check >
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading...
You must sign in or sign up to start the quiz.
You have to finish following quiz, to start this quiz:
Results
0 of 2 questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 points, (0)
Categories
- Not categorized 0%
- 1
- 2
- Answered
- Review
-
Question 1 of 2
1. Question
Question 1: What should be the next diagnostic step?
Correct
CORRECT ANSWER EXPLAINED BELOW Correct answer to Q1 is: Ultrasound guided biopsy of the liver lesion and discussion with the oncologist.
Incorrect
CORRECT ANSWER EXPLAINED BELOW Correct answer to Q1 is: Ultrasound guided biopsy of the liver lesion and discussion with the oncologist.
-
Question 2 of 2
2. Question
- Discussion
CEUS is the first-line imaging modality for the characterization of incidentally discovered focal liver lesions (FLL). CEUS can help in the clinical decision making also on the further clinical work-up. (1)
It is clear in this case that the liver lesions are malignant because they demonstrate wash-out in the late phase. The differential diagnoses are primary liver cancer or a secondary lesion. The FLL in this case has homogeneous arterial phase hyperenhancement and even the feeding artery could be distinguished in the very early arterial phase. This is characteristic of hepatocellular carcinoma, diagnostic if there is also cirrhosis, and some benign liver lesions like FNH and liver adenoma. The relatively late wash-out here is a sign of malignancy, but not specific for HCC. Differential diagnoses are liver metastases or intrahepatic cholangioarcinoma (ICC). It is important to note that multifocal disease may indicate metastases, but HCC and cholangiocarcinoma may also be multifocal.
Neuroendocrine tumors (NET) should also be taken into account in the differential diagnoses. They usually present as hyperenhancing lesions in the arterial phase due to their rich vascularization. Necrotic avascular areas may cause inhomogeneous enhancement in larger tumors. (2-3)
In our case the CT examination was inconclusive as well, because of the non-specific enhancement pattern of the liver lesions.
In cases of advanced metastatic malignancy of unknown primary origin and a good clinical status of the patient, it is always advisable to consider US-guided biopsy of a liver lesion to establish the diagnosis and guide the further treatment.
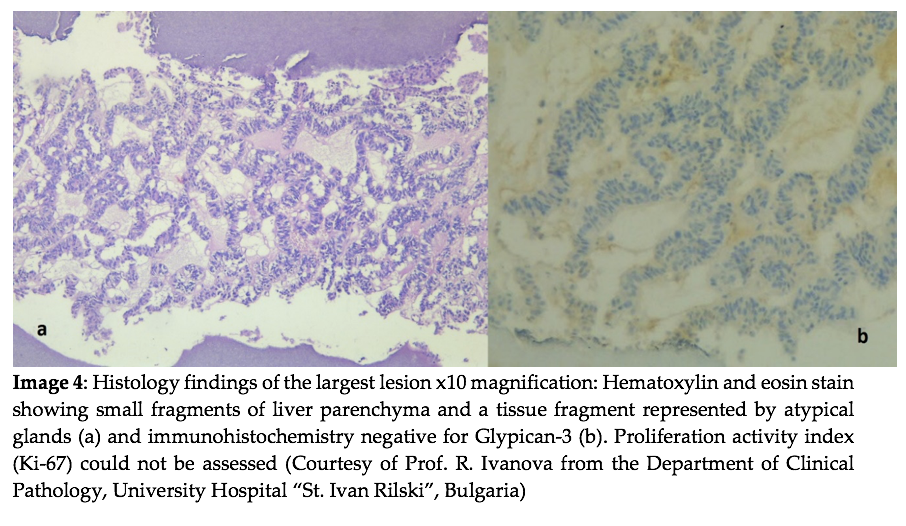
The histology and immunohistochemistry examination of the liver lesion in this case showed positive granular reaction in the peripheral liver parenchyma and positive reaction for Synaptophysin. PSA, CK-20, Hepatocyte and Amacr were all negative.
Question 2: What is the most likely diagnosis and should it be further specified?
Correct
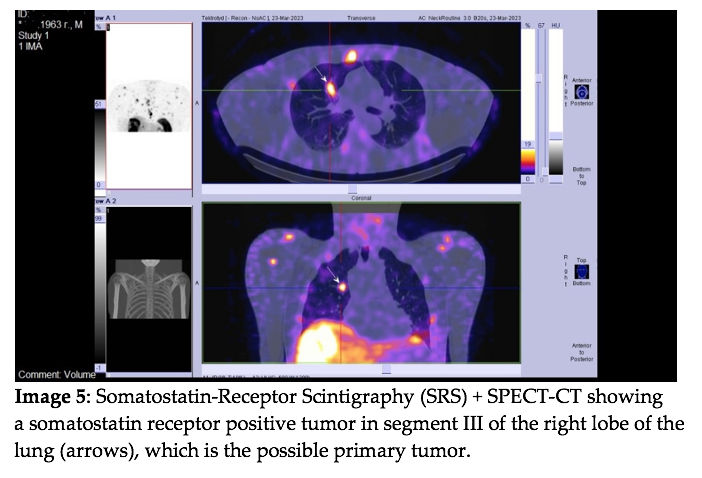
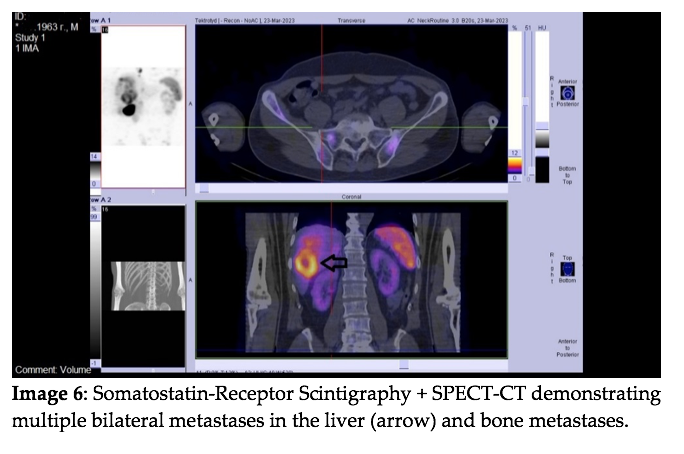
CORRECT ANSWER EXPLAINED BELOW Correct answer to Q2 is: Metastases from NET. The primary tumor origin should be assessed by Somatostatin Receptor Scintigraphy (SRS) or Cu/Ga-Dotatate PET/CT.
Additional discussion
In approximately 13% of patients who are diagnosed with NET, the primary site is not known. In such patients, the primary site is most frequently located in the intestine or the lung. Additional tests should be used to identify the primary tumor. These include immunohistochemistry of transcription factors (CDX-2, Islet-1, TTF-1), somatostatin receptor labelled scintigraphy or PET/CT (e.g. Ga-Dotatate PET/CT or Cu-Dotatate PET/CT), and upper and lower gastrointestinal endoscopy and optionally capsule endoscopy.
Histological examination of the metastases from NET should include conventional histology, immunohistochemistry for general neuroendocrine markers (i.e. synaptophysin and CgA) and determination of the proliferative activity by using Ki67 (4), which is a predictive factor for the aggressiveness of the tumor. In our case Ki67 could unfortunately not be established.Conclusion
CEUS is a helpful tool in differentiating between benign and malignant diagnoses in focal liver lesions especially in patients without previous malignancy.
Conflicts of Interest:
The authors declare no conflict of interest.
References:
1. Dietrich C; Nolsøe C, etc. Guidelines and Good Clinical Practice Recommendations for Contrast Enhanced Ultrasound (CEUS) in the liver – Update 2020. Ultraschall in Med 2020; 41: 562–585
2. Sidhu PS et al. The EFSUMB Guidelines and Recommendations for the Clinical Practice of Contrast-Enhanced Ultrasound (CEUS) in Non-Hepatic Applications: Update 2017 (Long Version). Ultraschall Med. 2018 Apr;39(2):e2-e44. English. doi: 10.1055/a-0586-1107. Epub 2018 Mar 6. PMID: 29510439.
3. Mörk H, Ignee A, Schuessler G, Ott M, Dietrich CF. Analysis of neuroendocrine tumour metastases in the liver using contrast enhanced ultrasonography. Scand J Gastroenterol. 2007 May;42(5):652-62. doi: 10.1080/00365520601021765. PMID: 17454888.
4. Pavel M, O’Toole D, Costa F, et al. ENETS Consensus Guidelines Update for the Management of Distant Metastatic Disease of Intestinal, Pancreatic, Bronchial Neuroendocrine Neoplasms (NEN) and NEN of Unknown Primary Site. Neuroendocrinology. 2016;103(2):172-85. doi: 10.1159/000443167. Epub 2016 Jan 5. PMID: 26731013.Incorrect
CORRECT ANSWER EXPLAINED BELOW Correct answer to Q2 is: Metastases from NET. The primary tumor origin should be assessed by Somatostatin Receptor Scintigraphy (SRS) or Cu/Ga-Dotatate PET/CT.
Additional discussion
In approximately 13% of patients who are diagnosed with NET, the primary site is not known. In such patients, the primary site is most frequently located in the intestine or the lung. Additional tests should be used to identify the primary tumor. These include immunohistochemistry of transcription factors (CDX-2, Islet-1, TTF-1), somatostatin receptor labelled scintigraphy or PET/CT (e.g. Ga-Dotatate PET/CT or Cu-Dotatate PET/CT), and upper and lower gastrointestinal endoscopy and optionally capsule endoscopy.
Histological examination of the metastases from NET should include conventional histology, immunohistochemistry for general neuroendocrine markers (i.e. synaptophysin and CgA) and determination of the proliferative activity by using Ki67 (4), which is a predictive factor for the aggressiveness of the tumor. In our case Ki67 could unfortunately not be established.Conclusion
CEUS is a helpful tool in differentiating between benign and malignant diagnoses in focal liver lesions especially in patients without previous malignancy.
Conflicts of Interest:
The authors declare no conflict of interest.
References:
1. Dietrich C; Nolsøe C, etc. Guidelines and Good Clinical Practice Recommendations for Contrast Enhanced Ultrasound (CEUS) in the liver – Update 2020. Ultraschall in Med 2020; 41: 562–585
2. Sidhu PS et al. The EFSUMB Guidelines and Recommendations for the Clinical Practice of Contrast-Enhanced Ultrasound (CEUS) in Non-Hepatic Applications: Update 2017 (Long Version). Ultraschall Med. 2018 Apr;39(2):e2-e44. English. doi: 10.1055/a-0586-1107. Epub 2018 Mar 6. PMID: 29510439.
3. Mörk H, Ignee A, Schuessler G, Ott M, Dietrich CF. Analysis of neuroendocrine tumour metastases in the liver using contrast enhanced ultrasonography. Scand J Gastroenterol. 2007 May;42(5):652-62. doi: 10.1080/00365520601021765. PMID: 17454888.
4. Pavel M, O’Toole D, Costa F, et al. ENETS Consensus Guidelines Update for the Management of Distant Metastatic Disease of Intestinal, Pancreatic, Bronchial Neuroendocrine Neoplasms (NEN) and NEN of Unknown Primary Site. Neuroendocrinology. 2016;103(2):172-85. doi: 10.1159/000443167. Epub 2016 Jan 5. PMID: 26731013.