Case of the month September 2024 – 26-week prenatal ultrasound: anechoic, cystic structure next to the midline of the brain. What do you think?
September 4, 2024
Case of the month November 2024: Sudden abdominal pain
November 19, 2024Maryla Kuczyńska 1*, Anna Drelich-Zbroja 1
1 Department of Interventional Radiology and Neuroradiology, Medical University of Lublin, Lublin, Poland; zaklad.radiologii.zabiegowej@spsk4.lublin.pl
* Correspondence: maryla.kuczynska@gmail.com
Clinical history
An 80-year-old female was referred for ultrasound of the neck due to a palpable, indolent lesion of the right mandibular angle – possibly related to the salivary (parotid/submandibular) gland. The patient reported progressive, visible enlargement of the lesion over 12 months. She was on permanent rivaroxaban treatment due to atrial fibrillation, and had a history of a car accident (with head and neck contusion) a year prior to the ultrasound examination.
Image
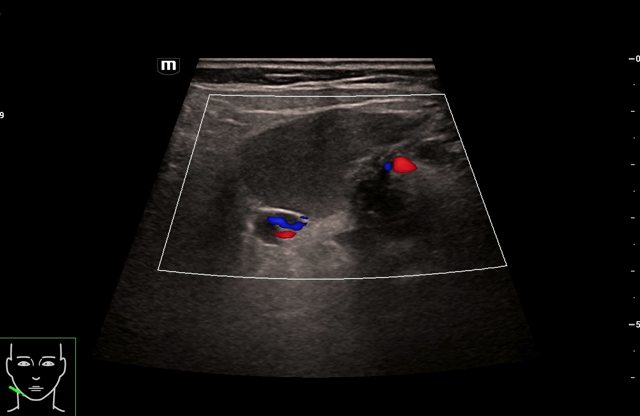
Video 1: CEUS depicts slow inflow of contrast from the posterior wall of the lesion, particularly seen when external compression is applied to the surrounding tissue using the probe. Additionally, spontaneous filling is seen following compression from pulsation of nearby arteries.
Quiz-summary
0 of 1 questions completed
Questions:
- 1
Information
View the October Case below, answer the question and then click check >
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading...
You must sign in or sign up to start the quiz.
You have to finish following quiz, to start this quiz:
Results
0 of 1 questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 points, (0)
Categories
- Not categorized 0%
- 1
- Answered
- Review
-
Question 1 of 1
1. Question
Question: Given the B-mode, Doppler US and CEUS appearance, what is the most likely diagnosis?
Correct
CORRECT ANSWER EXPLAINED BELOW Correct answer is: External jugular venous aneurysm.
Discussion
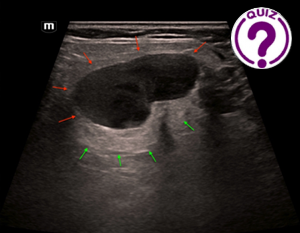
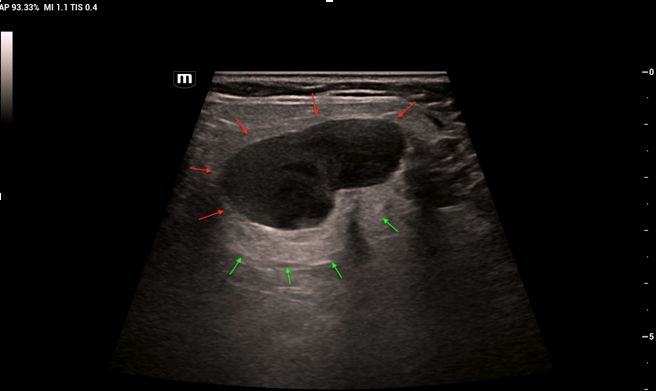
The lesion presented as well circumscribed, hypoechoic, rather homogenous, possibly cystic in nature with a content of high viscosity, related to the parotid gland. Some degree of posterior acoustic enhancement was visible. When slightly compressed/massaged with the ultrasound probe, the internal content of the lesion showed some degree of movement; the same was visible with arterial pulsation. As the lesion showed no overt flow signals on Doppler scanning, CEUS examination was performed.
Additional images / videos
Additional Discussion
Progressive filling-in of the lesion suggested a vascular origin. A branch of the ECA is immediately seen in the early arterial phase just posterior to the lesion (red arrows), with no evidence of direct relation (ie. no early arterial inflow to the lesion) – excluding the possibility of a pseudoaneurysm. After a few seconds the vein (green arrows) showing on the posterior border of the lesion is visible, supplying it with consecutive “jets” of enhancement.
Given the location, and solely based on the classic ultrasound appereance – the diagnostic differentials should include pleomorphic adenoma (the most common tumour of the salivary glands). This tumor would show some degree of heterogeneity and rather prominent acoustic enhancement at the posterior wall; however, no movement of the internal contents should be visible – which changes the diagnosis to cystic lesions. In this case, a second branchial cleft cyst would be a possibility. However, no enhancement should be seen with CEUS as the cyst is avascular. Given the progressive filling-in of the lesion, a vascular pathology should be taken into consideration. Lack of Doppler signal along with the CEUS enhancement pattern are atypical for arterial aneurysms, and so the remaining alternative is a venous ectatic lesion.
Further Images
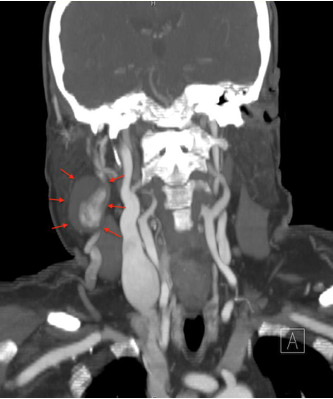
Image 4: Maximum intensity projection (MIP) reconstruction of the CT venous phase depicting a partially filling aneurysmal lesion in relation to the external jugular vein, confirming the diagnosis from CEUS.
Conclusion
Aneurysms of the external jugular vein are very rare entities. They may be congenital, iatrogenic (complication from head and neck surgery), or secondary to trauma or chronic disease (atrial fibrillation, hypertension). In the majority of cases, external jugular vein aneurysms remain asymptomatic, however, infrequently they may be complicated by thrombosis or pulmonary embolism. If large in size, they may cause compression to adjacent structures.
CEUS is a readily available problem solving tool in this regard.
Conflicts of Interest:
The authors declare no conflict of interest.
References
- Mittal MK, Malik A, Sureka B, Thukral BB. Cystic masses of neck: A pictorial review. Indian J Radiol Imaging. 2012;22(4):334-43.
- Nucera M, Meuli L, Janka H, Schindewolf M, Schmidli J, Makaloski V. Comprehensive review with pooled analysis on external and internal jugular vein aneurysm. J Vasc Surg Venous Lymphat Disord. 2022;10(3):778-785.
- Parashi HS, Rawekar KH, Joshi MM, Namdev HS, Jadhao MR, Bhosle KN. Saccular aneurysm of external jugular vein with partial thrombosis. Asian Cardiovascular and Thoracic Annals. 2018;26(8):625-627.
- Kovacs T, El Haddi S, Lee WA. Internal jugular venous aneurysm-A report of two cases with literature review. J Vasc Surg Cases Innov Tech. 2020;6(3):326-330.
- Chapman DR, Ho RE, Gangemi A. A case report of a rare, spontaneous external jugular vein aneurysm. International Journal of Surgery Case Reports. 2018; 52: 8-10.
- Boutakioute B, Benzalim M, Chehboun A, et al. Spontaneous external jugular vein pseudoaneurysm: A rare cause of neck swelling. Radiology Case Reports. 2022; 17: 4790-4794.
Incorrect
CORRECT ANSWER EXPLAINED BELOW Correct answer is: External jugular venous aneurysm.
Discussion
The lesion presented as well circumscribed, hypoechoic, rather homogenous, possibly cystic in nature with a content of high viscosity, related to the parotid gland. Some degree of posterior acoustic enhancement was visible. When slightly compressed/massaged with the ultrasound probe, the internal content of the lesion showed some degree of movement; the same was visible with arterial pulsation. As the lesion showed no overt flow signals on Doppler scanning, CEUS examination was performed.
Additional images / videos
Additional Discussion
Progressive filling-in of the lesion suggested a vascular origin. A branch of the ECA is immediately seen in the early arterial phase just posterior to the lesion (red arrows), with no evidence of direct relation (ie. no early arterial inflow to the lesion) – excluding the possibility of a pseudoaneurysm. After a few seconds the vein (green arrows) showing on the posterior border of the lesion is visible, supplying it with consecutive “jets” of enhancement.
Given the location, and solely based on the classic ultrasound appereance – the diagnostic differentials should include pleomorphic adenoma (the most common tumour of the salivary glands). This tumor would show some degree of heterogeneity and rather prominent acoustic enhancement at the posterior wall; however, no movement of the internal contents should be visible – which changes the diagnosis to cystic lesions. In this case, a second branchial cleft cyst would be a possibility. However, no enhancement should be seen with CEUS as the cyst is avascular. Given the progressive filling-in of the lesion, a vascular pathology should be taken into consideration. Lack of Doppler signal along with the CEUS enhancement pattern are atypical for arterial aneurysms, and so the remaining alternative is a venous ectatic lesion.
Further Images
Image 4: Maximum intensity projection (MIP) reconstruction of the CT venous phase depicting a partially filling aneurysmal lesion in relation to the external jugular vein, confirming the diagnosis from CEUS.
Conclusion
Aneurysms of the external jugular vein are very rare entities. They may be congenital, iatrogenic (complication from head and neck surgery), or secondary to trauma or chronic disease (atrial fibrillation, hypertension). In the majority of cases, external jugular vein aneurysms remain asymptomatic, however, infrequently they may be complicated by thrombosis or pulmonary embolism. If large in size, they may cause compression to adjacent structures.
CEUS is a readily available problem solving tool in this regard.
Conflicts of Interest:
The authors declare no conflict of interest.
References
- Mittal MK, Malik A, Sureka B, Thukral BB. Cystic masses of neck: A pictorial review. Indian J Radiol Imaging. 2012;22(4):334-43.
- Nucera M, Meuli L, Janka H, Schindewolf M, Schmidli J, Makaloski V. Comprehensive review with pooled analysis on external and internal jugular vein aneurysm. J Vasc Surg Venous Lymphat Disord. 2022;10(3):778-785.
- Parashi HS, Rawekar KH, Joshi MM, Namdev HS, Jadhao MR, Bhosle KN. Saccular aneurysm of external jugular vein with partial thrombosis. Asian Cardiovascular and Thoracic Annals. 2018;26(8):625-627.
- Kovacs T, El Haddi S, Lee WA. Internal jugular venous aneurysm-A report of two cases with literature review. J Vasc Surg Cases Innov Tech. 2020;6(3):326-330.
- Chapman DR, Ho RE, Gangemi A. A case report of a rare, spontaneous external jugular vein aneurysm. International Journal of Surgery Case Reports. 2018; 52: 8-10.
- Boutakioute B, Benzalim M, Chehboun A, et al. Spontaneous external jugular vein pseudoaneurysm: A rare cause of neck swelling. Radiology Case Reports. 2022; 17: 4790-4794.