NCUG 20th Anniversary Webinar: Advances in Interventional Ultrasound
March 14, 2022
Echoes Issue No. 26 [December 2021]
April 7, 2022Stacey Thomas 1 & Martin Necas 1
1 Waikato Hospital, Hamilton, New Zealand; martin@antegrade.net
* Correspondence: martin@antegrade.net
Clinical History:
A 58-year-old male with polycythemia vera and probable progression to myelofibrosis (later confirmed by bone marrow biopsy) was referred for an abdominal ultrasound through the Haematology outpatient clinic. He reported anaemia, weight loss and recent episode of LUQ pain which was not investigated due to the patient living on a small Pacific island with limited medical facilities.
Quiz-summary
0 of 2 questions completed
Questions:
- 1
- 2
Information
View the April Case below, answer the question and then click check >
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading...
You must sign in or sign up to start the quiz.
You have to finish following quiz, to start this quiz:
Results
0 of 2 questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 points, (0)
Categories
- Not categorized 0%
- 1
- 2
- Answered
- Review
-
Question 1 of 2
1. Question
Question 1: Which imaging modality would you suggest for evaluation of the spleen prior to a stem cell transplant?
Correct
CORRECT ANSWER EXPLAINED BELOW Correct answer to Q1 is: Ultrasound
Incorrect
CORRECT ANSWER EXPLAINED BELOW Correct answer to Q1 is: Ultrasound
-
Question 2 of 2
2. Question
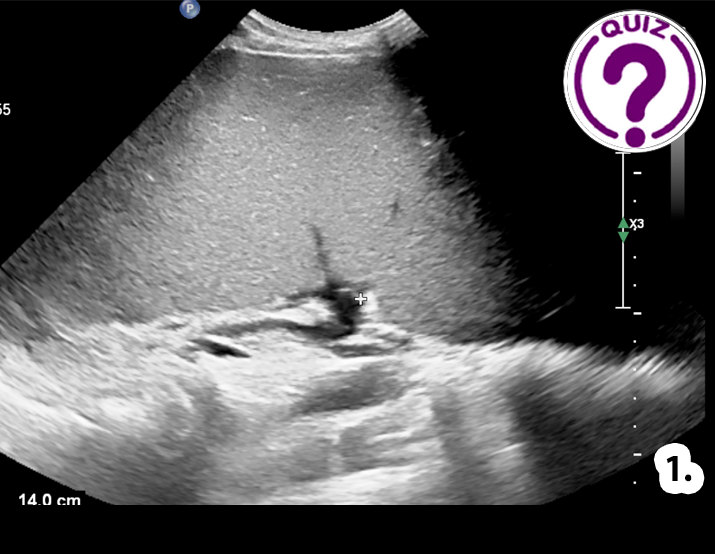
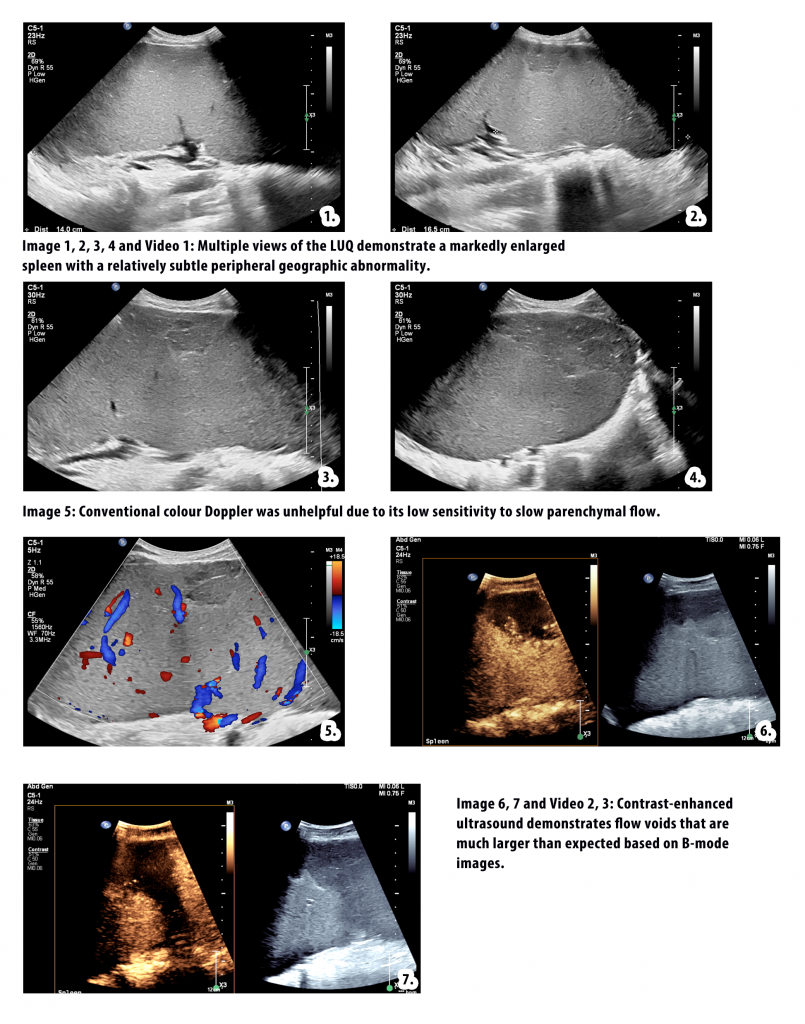
Conventional B-mode, colour Doppler and contrast-enhanced ultrasound (CEUS) images and videoclips of the spleen are shown. Imaging was performed on the Philips Epiq Elite system and the contrast agent used was Definity® (0.5ml single bolus).
Question 2: Based on the patient’s clinical history and ultrasound imaging, what is your diagnostic impression?
Correct
CORRECT ANSWER EXPLAINED BELOW Correct answer to Q2 is: Splenic infarcts
Discussion:
Massive splenomegaly is a common consequence of polycythemia vera and myelofibrosis (1). Secondary symptoms of splenomegaly can be detrimental to the quality of life of a patient. Massive splenomegaly can also contribute to portal hypertension due to increased splenic venous flow. Ischaemia of the spleen and painful infarcts may also occur (1).
On B-mode ultrasound a splenic infarct may appear as a wedge-shaped hypoechoic lesion with decreased vascularity on colour Doppler. The presence of hyperechoic linear bands within an infarct, ‘the bright band sign’, increases the specificity of a splenic infarct diagnosis (2). However, B-mode and colour Doppler have a low sensitivity for detecting infarcts because the infarcted splenic parenchyma may appear completely isoechoic with the surrounding normal tissue. The appearance of splenic infarcts can also be non-specific and indistinguishable from other splenic lesions (3,4).
Traditionally, CT was required for characterisation of splenic masses and effective detection of splenic infarcts (3). However, CT is relatively expensive, utilises ionising radiation and requires the use of nephrotoxic contrast agents. If a conventional ultrasound is non-specific and CT is required as a follow-up, this process may also result in diagnostic delays. CEUS has a high sensitivity for detecting splenic infarcts and can be performed immediately in conjunction with conventional ultrasound without the need to re-book the patient for a separate examination (3). CEUS is easy to implement and perform (5). The spleen is well suited to CEUS as it has similar properties to the liver in the retaining of contrast microbubbles (4). CEUS is considered as accurate as CT for diagnosing hypovascular splenic lesions (3).
The imaging appearance of a splenic infarct on CEUS is a persistently non-perfused area after a bolus of contrast is given (3,4). The typical wedge-shaped appearance of an infarct, pointing towards the hilum of the spleen (as shown in image 7 and videos 2 and 3) is a typical feature of large infarcts (4). Infarcts as small as 7mm are able to be detected using CEUS (3).
Splenic infarcts, abscesses and lacerations from trauma will all have a similar non-perfused appearance on CEUS. Clinical history and laboratory results are therefore important in distinguishing between these types of avascular splenic masses.
Conflicts of interest
“The authors declare no conflict of interest.”
References
- Tremblay D, Schwartz M, Bakst R, Patel R, Schiano T, Marina K, et al. Modern management of splenomegaly in patients with myelofibrosis. Annals of Hematology. 2020;99(7):1441–51.
- Llewellyn ME, Jeffrey RB, DiMaio MA, Olcott EW. The Sonographic “Bright Band Sign” of Splenic Infarction. Journal of Ultrasound in Medicine. 2014;33(6):929–38.
- Menozzi G, Maccabruni V, Gabbi E, Magnani G, Garlassi E. Evaluation with contrast ultrasound of the prevalence of splenic infarction in left-sided infective endocarditis. J Ultrasound. 2014;18(3):223–7.
- Omar A, Freeman S. Contrast-enhanced ultrasound of the spleen. Ultrasound. 2016 Feb;24(1):41–9.
- Necas M, Keating J, Abbott G, Curtis N, de Ryke R, Hill G. How to set-up and perform contrast-enhanced ultrasound. Australasian Journal of Ultrasound in Medicine. 2019;22(2):86–95.
Incorrect
CORRECT ANSWER EXPLAINED BELOW Correct answer to Q2 is: Splenic infarcts
Discussion:
Massive splenomegaly is a common consequence of polycythemia vera and myelofibrosis (1). Secondary symptoms of splenomegaly can be detrimental to the quality of life of a patient. Massive splenomegaly can also contribute to portal hypertension due to increased splenic venous flow. Ischaemia of the spleen and painful infarcts may also occur (1).
On B-mode ultrasound a splenic infarct may appear as a wedge-shaped hypoechoic lesion with decreased vascularity on colour Doppler. The presence of hyperechoic linear bands within an infarct, ‘the bright band sign’, increases the specificity of a splenic infarct diagnosis (2). However, B-mode and colour Doppler have a low sensitivity for detecting infarcts because the infarcted splenic parenchyma may appear completely isoechoic with the surrounding normal tissue. The appearance of splenic infarcts can also be non-specific and indistinguishable from other splenic lesions (3,4).
Traditionally, CT was required for characterisation of splenic masses and effective detection of splenic infarcts (3). However, CT is relatively expensive, utilises ionising radiation and requires the use of nephrotoxic contrast agents. If a conventional ultrasound is non-specific and CT is required as a follow-up, this process may also result in diagnostic delays. CEUS has a high sensitivity for detecting splenic infarcts and can be performed immediately in conjunction with conventional ultrasound without the need to re-book the patient for a separate examination (3). CEUS is easy to implement and perform (5). The spleen is well suited to CEUS as it has similar properties to the liver in the retaining of contrast microbubbles (4). CEUS is considered as accurate as CT for diagnosing hypovascular splenic lesions (3).
The imaging appearance of a splenic infarct on CEUS is a persistently non-perfused area after a bolus of contrast is given (3,4). The typical wedge-shaped appearance of an infarct, pointing towards the hilum of the spleen (as shown in image 7 and videos 2 and 3) is a typical feature of large infarcts (4). Infarcts as small as 7mm are able to be detected using CEUS (3).
Splenic infarcts, abscesses and lacerations from trauma will all have a similar non-perfused appearance on CEUS. Clinical history and laboratory results are therefore important in distinguishing between these types of avascular splenic masses.
Conflicts of interest
“The authors declare no conflict of interest.”
References
- Tremblay D, Schwartz M, Bakst R, Patel R, Schiano T, Marina K, et al. Modern management of splenomegaly in patients with myelofibrosis. Annals of Hematology. 2020;99(7):1441–51.
- Llewellyn ME, Jeffrey RB, DiMaio MA, Olcott EW. The Sonographic “Bright Band Sign” of Splenic Infarction. Journal of Ultrasound in Medicine. 2014;33(6):929–38.
- Menozzi G, Maccabruni V, Gabbi E, Magnani G, Garlassi E. Evaluation with contrast ultrasound of the prevalence of splenic infarction in left-sided infective endocarditis. J Ultrasound. 2014;18(3):223–7.
- Omar A, Freeman S. Contrast-enhanced ultrasound of the spleen. Ultrasound. 2016 Feb;24(1):41–9.
- Necas M, Keating J, Abbott G, Curtis N, de Ryke R, Hill G. How to set-up and perform contrast-enhanced ultrasound. Australasian Journal of Ultrasound in Medicine. 2019;22(2):86–95.