Ultrasound the first line investigation in upper abdominal pain? ~ Dieter Nurnberg (Germany)
July 20, 2022
WFUMB / EFSUMB Students Webinar Series: 10 September 2022
September 12, 2022Roni Yoeli-Bik 1, Kathryn A. Mills 2, Jacques S. Abramowicz 3
1 University of Chicago ; ryoelibik@bsd.uchicago.edu
2 University of Chicago ; kmills6@bsd.uchicago.edu
3 University of Chicago ; jabramowicz@bsd.uchicago.edu
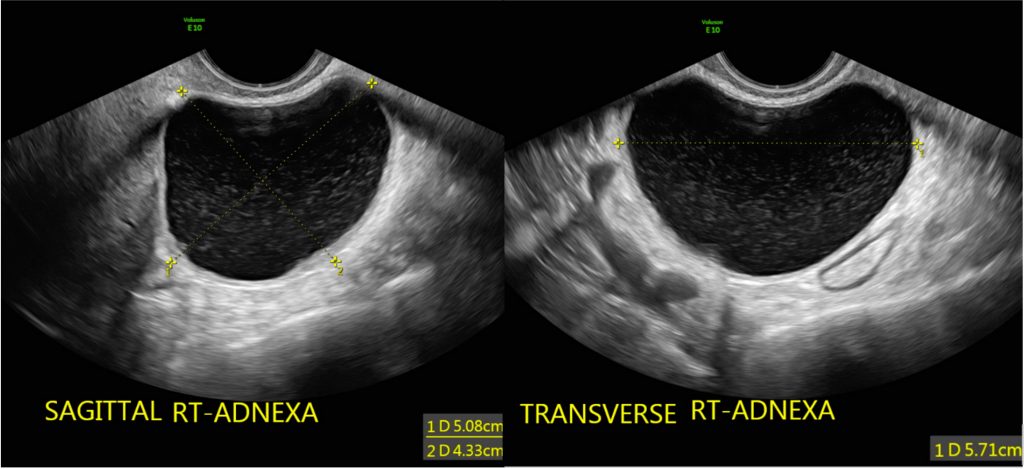
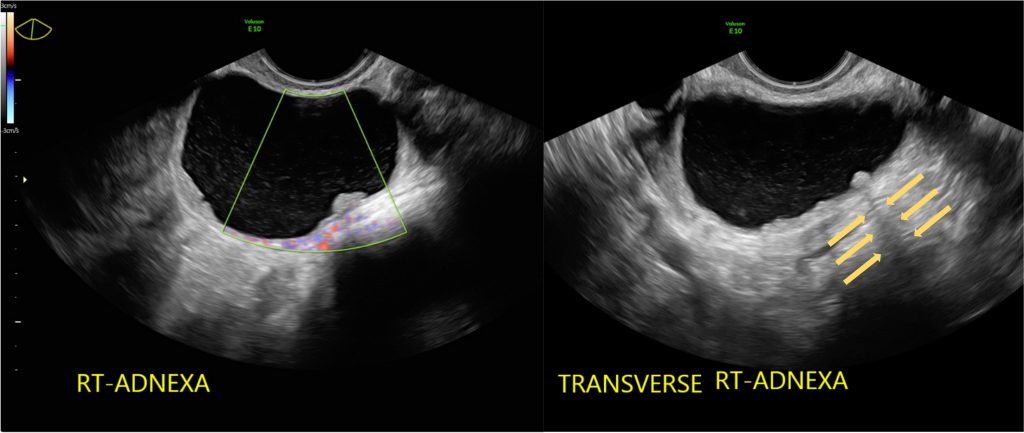
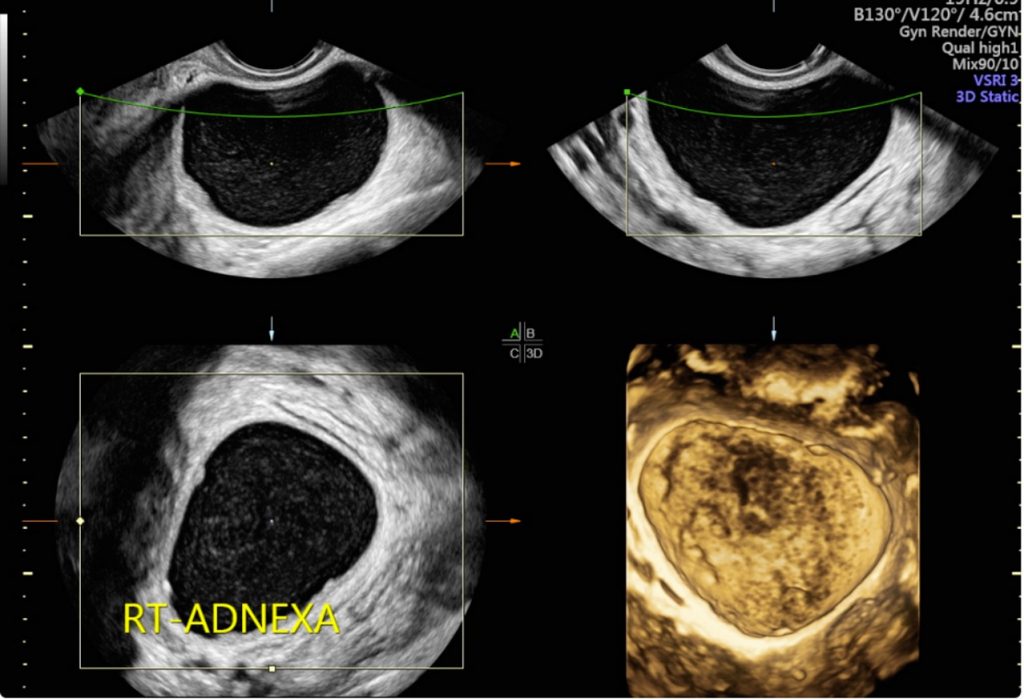
Clinical History
A 23-year-old, nulligravid female with polycystic ovary syndrome complained of right upper quadrant pain for a few months. A CT scan revealed gall stones and an incidental finding of a right adnexal mass, and she was referred to gynecology. She had regular menstrual cycles and denied a family history of breast, uterine, ovarian, or colorectal cancer. On physical examination, the patient appeared well, vital signs were normal, the abdomen was soft, and no mass was palpated. During the pelvic exam, a roughly 6 cm smooth mobile, non-tender mass palpated in her right adnexa. The rest of her physical exam was unremarkable. A transvaginal ultrasound scan was performed (images 1-3, video 1) and revealed a 5x4x6 cm right adnexal mass. Using IOTA (International Ovarian Tumor Analysis) criteria, the mass was characterized as a unilocular solid lesion with scattered low-level echoes, a color Doppler score of 1 (no flow), acoustic shadow present, and no ascites noted. Tumor markers (CA-125, bets HCG, AFP, Inhibin A/B, LDH) were within normal limits. Given these ultrasound findings, she was referred to gynecologic oncology for management. Options for observation of the mass with close serial ultrasound versus cystectomy were reviewed with the patient and her family, and she chose to proceed with operative management. Surgery was performed and revealed a 6 cm thin-walled paratubal cystic mass with multiple vessels traversing the walls of the mass. A right salpingectomy and paratubal cyst removal were completed and the specimens were sent to pathology. Post-operative management was unremarkable.
Images / Videos
Quiz-summary
0 of 1 questions completed
Questions:
- 1
Information
View the August Case below, answer the question and then click check >
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading...
You must sign in or sign up to start the quiz.
You have to finish following quiz, to start this quiz:
Results
0 of 1 questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 points, (0)
Categories
- Not categorized 0%
- 1
- Answered
- Review
-
Question 1 of 1
1. Question
Question: What is the most likely diagnosis?
Correct
CORRECT ANSWER EXPLAINED BELOW Correct answer is: Serous cystadenofibroma
Discussion
Pathology revealed the diagnosis to be serous cystadenofibroma. Cystadenofibroma, which are relatively rare benign ovarian tumors, contain dominant stromal proliferations that overshadow the epithelial element. When the stroma is highly cellular and fibrous, and forms large solid areas containing scattered glands or thick papillary projections, the tumor is called adenofibroma. If there is a cystic component, it is called cystadenofibroma (1). Cystadenofibromas occur in women of all ages, but most frequently in those between 40 and 60 years of age. The symptoms and signs associated with cystadenofibromas are nonspecific (1). The possibility of recognizing typical ultrasound features of these lesions is important as it can influence both patients’ and physicians’ decisions regarding management and treatment (1). Many cystadenofibromas contain papillary projections, and thus may be potentially confused with malignancies and borderline tumors, leading to surgical intervention (1-2).
By advancing the clinical management and pre-operative triage of patients with adnexal masses like cystadenofibroma, patient care and the burden on the healthcare system would vastly improve (3). Optimizing the referral of patients to a gynecologic oncologist in cases of suspected ovarian malignancies is critical, as patient prognosis is known to significantly improve when surgery is performed by a subspecialist; however, not every mass requires oncologic assessment, and most adnexal masses in premenopausal patients are benign (3). In addition, a more conservative approach, when applicable, could reduce risk for patients, as complication rates from surgery range from 2% to 15% (3). Ultrasound plays a crucial role in the pre-operative assessment of adnexal masses and is the best modality to differentiate between benign and malignant status (3-4). Efforts to improve clinical management and pre-operatively triage patterns would ultimately improve patient care (3).
Timor-Tritsch et al. described the “shadow sign” as a pathognomonic characteristic of cystadenofibromas. They showed that the presence of hyperechoic avascular shadowing nodules, in a typical unilocular or multilocular cyst with a thin avascular septa, is a reliable sign for cystadenofibromas (2). This ultrasound marker helps differentiate cystadenofibromas from borderline ovarian tumors and ovarian malignancies, which do not show this ultrasound feature (2).
The IOTA Simple Rules and ADNEX model are useful during the pre-operative assessment (3). These tools were developed for simplicity and can help the provider distinguish benign from malignant lesions, even in the hands of a non-expert (3-5). Using IOTA models, one can characterize the cystadenofibromas correctly (like in the presented case) since both the Simple Rules and the ADNEX models incorporate acoustic shadow as one of the parameters and, thus, help classify these lesions accurately (4-5).
Precise recognition of cystadenofibromas can potentially minimize unnecessary testing by computed tomography or magnetic resonance imaging, and, more importantly, will avoid unwarranted surgical intervention (2).
Conclusion
Cystadenofibromas are relatively rare benign ovarian tumors that may look malignant on the pre-operative assessment, leading to unnecessary surgical interventions and referrals to subspecialists. Using the “shadow sign” when conducting ultrasound can help distinguish and characterize lesions correctly. IOTA models, which incorporate acoustic shadow, can help properly classify these lesions as benign. Looking for the “shadow sign” and using the IOTA models will improve the correct diagnosis of cystadenofibroma, discriminating it from borderline tumors and ovarian cancer, therefore avoiding unnecessary cost and morbidity, and improving patient care.
Conflicts of Interest
The authors declare no conflict of interest
References
- Virgilio BA, De Blasis I, Sladkevicius P, Moro F, Zannoni GF, Arciuolo D, Mascilini F, Ciccarone F, Timmerman D, Kaijser J, Fruscio R. Imaging in gynecological disease (16): clinical and ultrasound characteristics of serous cystadenofibromas in adnexa. Ultrasound in Obstetrics & Gynecology. 2019 Dec;54(6):823-30.
- Timor‐Tritsch IE, Yoon E, Monteagudo A, Ciaffarano J, Brandon C, Mittal KR, Wallach RC, Boyd LR. Ultrasound and histopathologic correlation of ovarian cystadenofibromas: diagnostic value of the “shadow sign”. Journal of Ultrasound in Medicine. 2019 Nov;38(11):2973-8.
- Glanc P, Benacerraf B, Bourne T, Brown D, Coleman BG, Crum C, Dodge J, Levine D, Pavlik E, Timmerman D, Ueland FR, Wolfman W, Goldstein SR. First International Consensus Report on Adnexal Masses: Management Recommendations. J Ultrasound Med. 2017 May;36(5):849-863.
- Abramowicz JS, Timmerman D. Ovarian mass–differentiating benign from malignant: the value of the International Ovarian Tumor Analysis ultrasound rules. American journal of obstetrics and gynecology. 2017 Dec 1;217(6):652-60.
- Timmerman D, Ameye L, Fischerova D, Epstein E, Melis GB, Guerriero S, Van Holsbeke C, Savelli L, Fruscio R, Lissoni AA, Testa AC, Veldman J, Vergote I, Van Huffel S, Bourne T, Valentin L. Simple ultrasound rules to distinguish between benign and malignant adnexal masses before surgery: prospective validation by IOTA group. BMJ. 2010 Dec 14;341:c6839.
Incorrect
CORRECT ANSWER EXPLAINED BELOW Correct answer is: Serous cystadenofibroma
Discussion
Pathology revealed the diagnosis to be serous cystadenofibroma. Cystadenofibroma, which are relatively rare benign ovarian tumors, contain dominant stromal proliferations that overshadow the epithelial element. When the stroma is highly cellular and fibrous, and forms large solid areas containing scattered glands or thick papillary projections, the tumor is called adenofibroma. If there is a cystic component, it is called cystadenofibroma (1). Cystadenofibromas occur in women of all ages, but most frequently in those between 40 and 60 years of age. The symptoms and signs associated with cystadenofibromas are nonspecific (1). The possibility of recognizing typical ultrasound features of these lesions is important as it can influence both patients’ and physicians’ decisions regarding management and treatment (1). Many cystadenofibromas contain papillary projections, and thus may be potentially confused with malignancies and borderline tumors, leading to surgical intervention (1-2).
By advancing the clinical management and pre-operative triage of patients with adnexal masses like cystadenofibroma, patient care and the burden on the healthcare system would vastly improve (3). Optimizing the referral of patients to a gynecologic oncologist in cases of suspected ovarian malignancies is critical, as patient prognosis is known to significantly improve when surgery is performed by a subspecialist; however, not every mass requires oncologic assessment, and most adnexal masses in premenopausal patients are benign (3). In addition, a more conservative approach, when applicable, could reduce risk for patients, as complication rates from surgery range from 2% to 15% (3). Ultrasound plays a crucial role in the pre-operative assessment of adnexal masses and is the best modality to differentiate between benign and malignant status (3-4). Efforts to improve clinical management and pre-operatively triage patterns would ultimately improve patient care (3).
Timor-Tritsch et al. described the “shadow sign” as a pathognomonic characteristic of cystadenofibromas. They showed that the presence of hyperechoic avascular shadowing nodules, in a typical unilocular or multilocular cyst with a thin avascular septa, is a reliable sign for cystadenofibromas (2). This ultrasound marker helps differentiate cystadenofibromas from borderline ovarian tumors and ovarian malignancies, which do not show this ultrasound feature (2).
The IOTA Simple Rules and ADNEX model are useful during the pre-operative assessment (3). These tools were developed for simplicity and can help the provider distinguish benign from malignant lesions, even in the hands of a non-expert (3-5). Using IOTA models, one can characterize the cystadenofibromas correctly (like in the presented case) since both the Simple Rules and the ADNEX models incorporate acoustic shadow as one of the parameters and, thus, help classify these lesions accurately (4-5).
Precise recognition of cystadenofibromas can potentially minimize unnecessary testing by computed tomography or magnetic resonance imaging, and, more importantly, will avoid unwarranted surgical intervention (2).
Conclusion
Cystadenofibromas are relatively rare benign ovarian tumors that may look malignant on the pre-operative assessment, leading to unnecessary surgical interventions and referrals to subspecialists. Using the “shadow sign” when conducting ultrasound can help distinguish and characterize lesions correctly. IOTA models, which incorporate acoustic shadow, can help properly classify these lesions as benign. Looking for the “shadow sign” and using the IOTA models will improve the correct diagnosis of cystadenofibroma, discriminating it from borderline tumors and ovarian cancer, therefore avoiding unnecessary cost and morbidity, and improving patient care.
Conflicts of Interest
The authors declare no conflict of interest
References
- Virgilio BA, De Blasis I, Sladkevicius P, Moro F, Zannoni GF, Arciuolo D, Mascilini F, Ciccarone F, Timmerman D, Kaijser J, Fruscio R. Imaging in gynecological disease (16): clinical and ultrasound characteristics of serous cystadenofibromas in adnexa. Ultrasound in Obstetrics & Gynecology. 2019 Dec;54(6):823-30.
- Timor‐Tritsch IE, Yoon E, Monteagudo A, Ciaffarano J, Brandon C, Mittal KR, Wallach RC, Boyd LR. Ultrasound and histopathologic correlation of ovarian cystadenofibromas: diagnostic value of the “shadow sign”. Journal of Ultrasound in Medicine. 2019 Nov;38(11):2973-8.
- Glanc P, Benacerraf B, Bourne T, Brown D, Coleman BG, Crum C, Dodge J, Levine D, Pavlik E, Timmerman D, Ueland FR, Wolfman W, Goldstein SR. First International Consensus Report on Adnexal Masses: Management Recommendations. J Ultrasound Med. 2017 May;36(5):849-863.
- Abramowicz JS, Timmerman D. Ovarian mass–differentiating benign from malignant: the value of the International Ovarian Tumor Analysis ultrasound rules. American journal of obstetrics and gynecology. 2017 Dec 1;217(6):652-60.
- Timmerman D, Ameye L, Fischerova D, Epstein E, Melis GB, Guerriero S, Van Holsbeke C, Savelli L, Fruscio R, Lissoni AA, Testa AC, Veldman J, Vergote I, Van Huffel S, Bourne T, Valentin L. Simple ultrasound rules to distinguish between benign and malignant adnexal masses before surgery: prospective validation by IOTA group. BMJ. 2010 Dec 14;341:c6839.