WFUMB / EFSUMB Students Webinar Series: 02 September 2021
September 6, 2021
Case of the Month October 2021- Preterm neonate with abdominal distention and clinical decompensation
October 1, 2021Sofie Bech Andersen1,*
1 Department of Radiology, Rigshospitalet, DK-2100 Copenhagen, Denmark
* Correspondence: anne.sofie.bech.andersen@regionh.dk
Clinical History:
A 54-year old female with a past medical history of rheumatoid arthritis, a hiatus hernia, and appendectomy as a child, presented with intermittent upper abdominal pain and vomiting. The abdominal pain had occurred every 2nd to 3rd month during the past years, each time lasting roughly 3 days. The pain radiated to the back. No fever, weight loss or alterations in feces and urine was reported.
A physical exam revealed the patient’s abdomen soft and non-tender with no palpable masses.
With a clinical suspicion of gall stones, an abdominal ultrasound examination was requested and performed.
Quiz-summary
0 of 2 questions completed
Questions:
- 1
- 2
Information
View the September Case below, answer the question and then click check >
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading...
You must sign in or sign up to start the quiz.
You have to finish following quiz, to start this quiz:
Results
0 of 2 questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 points, (0)
Categories
- Not categorized 0%
- 1
- 2
- Answered
- Review
-
Question 1 of 2
1. Question
Correct
CORRECT ANSWER EXPLAINED BELOW Correct answer to Q1 is: Liver metastasis
Incorrect
CORRECT ANSWER EXPLAINED BELOW Correct answer to Q1 is: Liver metastasis
-
Question 2 of 2
2. Question
Further findings
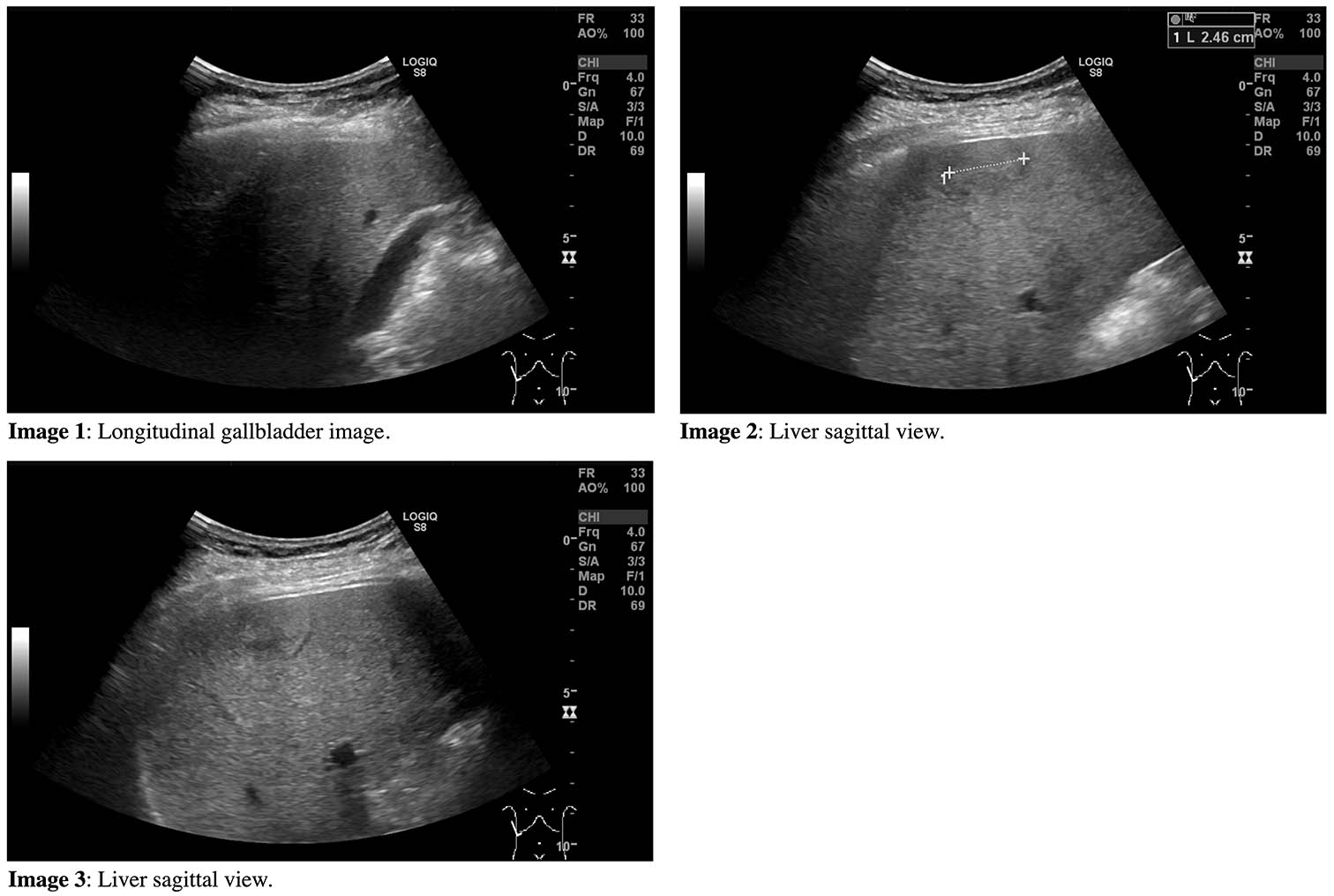
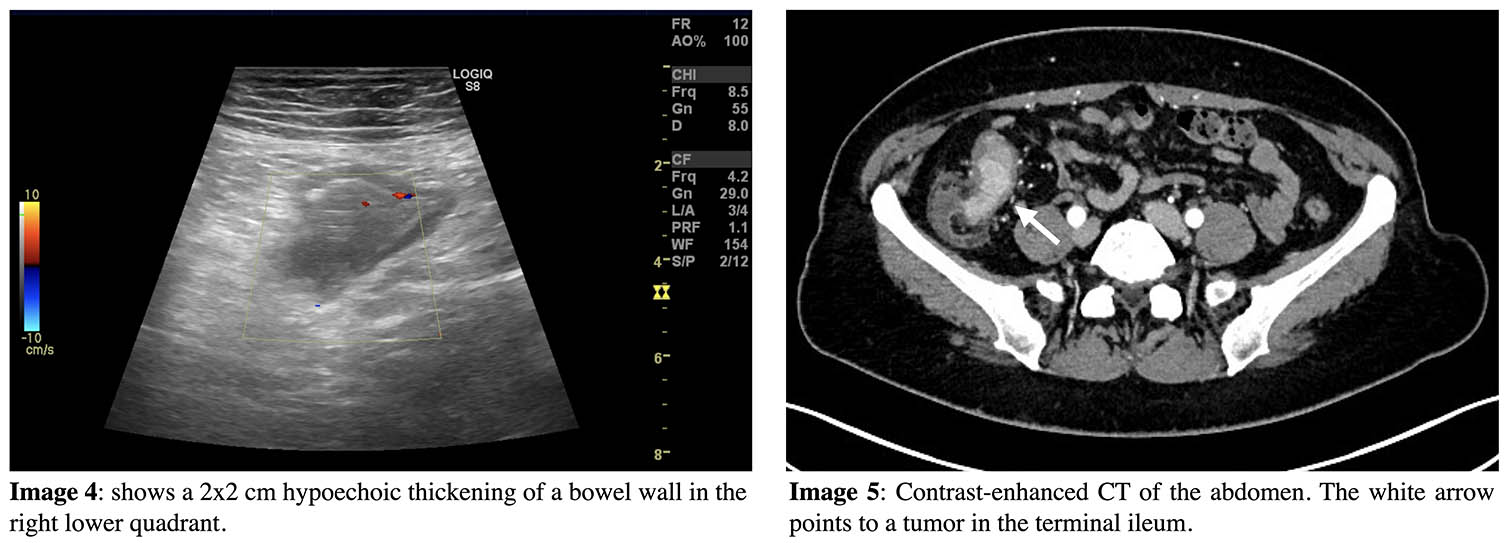
The ultrasound examination of the liver revealed mild steatosis and a 2.5 cm isoechoic mass with a hypoechoic halo in the right liver lobe. No stones in the gall bladder and no cholestasis. Normal examination of pancreas, spleen and kidneys. The ultrasound examination also revealed a bowel wall thickening, probably in the ascending colon, near the coecum (Image 4). To follow up, a CT scan of the thorax and abdomen was performed. It revealed a tumor in the terminal ileum (Image 5).
Ultrasound examination of the colon and abdominal CT
Question 2: What is now the most likely diagnosis for the liver tumor?
Correct
CORRECT ANSWER EXPLAINED BELOW Correct answer to Q2 is: Liver metastasis from intestinal cancer
Discussion:
A hypoechoic halo, which is a hypoechoic rim in the periphery of a lesion, is a concerning feature of liver masses. It has been shown to be highly indicative of malignancy compared with lesions without halo (1). In this case, contrast-enhanced ultrasound was unavailable, but it might have revealed more lesions, and would probably have determined the malignant origin. As liver metastases most often originate from the colon, the colon was carefully inspected during the ultrasound examination, and this revealed intestinal wall thickening in the right lower quadrant. Based on these findings, a thoracic and abdominal CT scan and a colonoscopy were recommended.
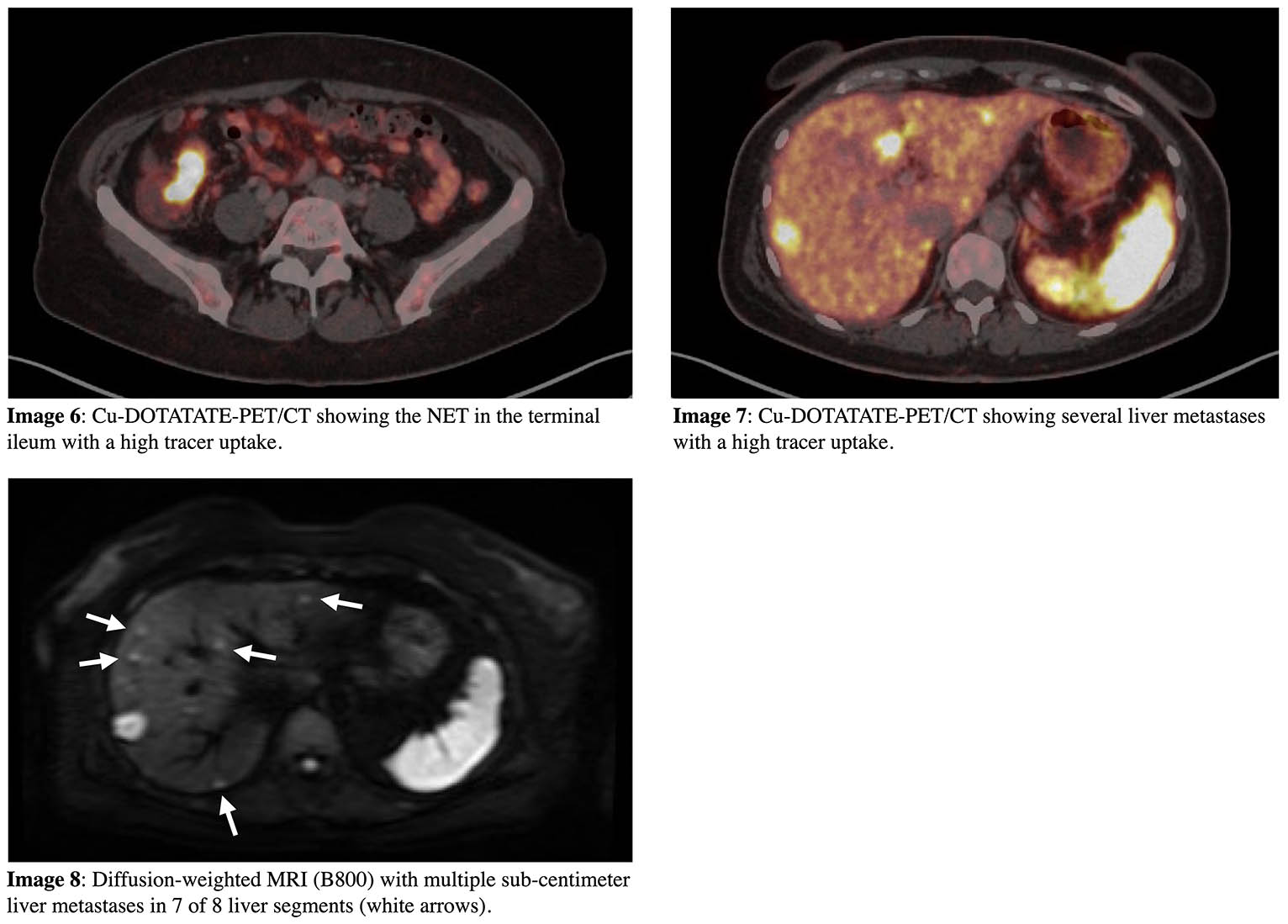
The CT scan revealed a tumor in the terminal ileum. After the CT scan, a colonoscopy with biopsies from the terminal ileum was performed. The following histopathology determined the mass to be a neuroendocrine tumor (NET) with a Ki-67 proliferative index of 3%, meaning it was an intermediate-grade tumor (2). The currently recommended examinations for imaging of patients with NETs include a combination of molecular and morphologic imaging. Therefore, a Cu-DOTATATE-PET/CT (somatostatin analogue radiotracer) was performed to determine malignant spread (Image 6 and 7). The scan showed the tumor in the terminal ileum and several liver metastases, at least 20. Diffusion-weighted MRI has proven very sensitive for detection of liver metastases (3), and to determine the possibility of liver resection, it was also performed. Unfortunately, the MRI revealed multiple sub-centimeter metastases in all liver segments except segment 1, making them irresectable (Image 8).
This patient had a mid-gut NET with liver metastases, but she did not present with the typical carcinoid syndrome (i.e., flushing, diarrhea, tachycardia, or hypotension, bronchospasms, and right-sided heart failure), even though mid-gut NETs with metastases are among the most common tumors to cause the syndrome. However, only roughly 10% of patients with NETs experience typical carcinoid symptoms. It is more typical for these patients to present with weak and unspecific symptoms, and many small bowel NETs are found by coincidence (4,5). Among symptomatic patients with small bowel NETs, abdominal pain is one of the most common initial symptoms. In addition, intermittent obstruction occurs in approximately 25% of small bowel NETs. In this case, the patient’s symptoms with intermittent upper abdominal pain and vomiting could have been caused by intermittent bowel obstruction.
In conclusion, one should look carefully at the other intraabdominal organs and intestines when liver metastases are seen or suspected. In female patients an origin in the breasts should also be considered.
Conflicts of interest
“The authors declare no conflict of interest.”
References
- Wernecke, K.; Vassallo, P.; Bick, U.; Diederich, S.; Peters, P.E. The distinction between benign and malignant liver tumors on sonography: Value of a hypoechoic halo. Am. J. Roentgenol. 1992, 159, 1005–1009.
- Nagtegaal, I.D.; Odze, R.D.; Klimstra, D.; Paradis, V.; Rugge, M.; Schirmacher, P.; Washington, K.M.; Carneiro, F.; Cree, I.A. The 2019 WHO classification of tumours of the digestive system. Histopathology 2020, 76, 182–188.
- d’Assignies, G.; Fina, P.; Bruno, O.; Vullierme, M.P.; Tubach, F.; Paradis, V.; Sauvanet, A.; Ruszniewski, P.; Vilgrain, V. High sensitivity of diffusion-weighted mr imaging for the detection of liver metastases from neuroendocrine tumors : Comparison with t2-weighted and dynamic gadolinium-enhanced mr imaging. Radiology 2013, 268, 390–399.
- Kulke, M.H.; Mayer, R.J. Carcinoid tumors. N. Engl. J. Med. 1999, 340, 858–68.
- Cheung, V.T.F.; Khan, M.S. A guide to midgut neuroendocrine tumours (NETs) and carcinoid syndrome. Frontline Gastroenterol. 2015, 6, 264–269.
Incorrect
CORRECT ANSWER EXPLAINED BELOW Correct answer to Q2 is: Liver metastasis from intestinal cancer
Discussion:
A hypoechoic halo, which is a hypoechoic rim in the periphery of a lesion, is a concerning feature of liver masses. It has been shown to be highly indicative of malignancy compared with lesions without halo (1). In this case, contrast-enhanced ultrasound was unavailable, but it might have revealed more lesions, and would probably have determined the malignant origin. As liver metastases most often originate from the colon, the colon was carefully inspected during the ultrasound examination, and this revealed intestinal wall thickening in the right lower quadrant. Based on these findings, a thoracic and abdominal CT scan and a colonoscopy were recommended.
The CT scan revealed a tumor in the terminal ileum. After the CT scan, a colonoscopy with biopsies from the terminal ileum was performed. The following histopathology determined the mass to be a neuroendocrine tumor (NET) with a Ki-67 proliferative index of 3%, meaning it was an intermediate-grade tumor (2). The currently recommended examinations for imaging of patients with NETs include a combination of molecular and morphologic imaging. Therefore, a Cu-DOTATATE-PET/CT (somatostatin analogue radiotracer) was performed to determine malignant spread (Image 6 and 7). The scan showed the tumor in the terminal ileum and several liver metastases, at least 20. Diffusion-weighted MRI has proven very sensitive for detection of liver metastases (3), and to determine the possibility of liver resection, it was also performed. Unfortunately, the MRI revealed multiple sub-centimeter metastases in all liver segments except segment 1, making them irresectable (Image 8).
This patient had a mid-gut NET with liver metastases, but she did not present with the typical carcinoid syndrome (i.e., flushing, diarrhea, tachycardia, or hypotension, bronchospasms, and right-sided heart failure), even though mid-gut NETs with metastases are among the most common tumors to cause the syndrome. However, only roughly 10% of patients with NETs experience typical carcinoid symptoms. It is more typical for these patients to present with weak and unspecific symptoms, and many small bowel NETs are found by coincidence (4,5). Among symptomatic patients with small bowel NETs, abdominal pain is one of the most common initial symptoms. In addition, intermittent obstruction occurs in approximately 25% of small bowel NETs. In this case, the patient’s symptoms with intermittent upper abdominal pain and vomiting could have been caused by intermittent bowel obstruction.
In conclusion, one should look carefully at the other intraabdominal organs and intestines when liver metastases are seen or suspected. In female patients an origin in the breasts should also be considered.
Conflicts of interest
“The authors declare no conflict of interest.”
References
- Wernecke, K.; Vassallo, P.; Bick, U.; Diederich, S.; Peters, P.E. The distinction between benign and malignant liver tumors on sonography: Value of a hypoechoic halo. Am. J. Roentgenol. 1992, 159, 1005–1009.
- Nagtegaal, I.D.; Odze, R.D.; Klimstra, D.; Paradis, V.; Rugge, M.; Schirmacher, P.; Washington, K.M.; Carneiro, F.; Cree, I.A. The 2019 WHO classification of tumours of the digestive system. Histopathology 2020, 76, 182–188.
- d’Assignies, G.; Fina, P.; Bruno, O.; Vullierme, M.P.; Tubach, F.; Paradis, V.; Sauvanet, A.; Ruszniewski, P.; Vilgrain, V. High sensitivity of diffusion-weighted mr imaging for the detection of liver metastases from neuroendocrine tumors : Comparison with t2-weighted and dynamic gadolinium-enhanced mr imaging. Radiology 2013, 268, 390–399.
- Kulke, M.H.; Mayer, R.J. Carcinoid tumors. N. Engl. J. Med. 1999, 340, 858–68.
- Cheung, V.T.F.; Khan, M.S. A guide to midgut neuroendocrine tumours (NETs) and carcinoid syndrome. Frontline Gastroenterol. 2015, 6, 264–269.