The Australasian Society for Ultrasound in Medicine Congress (ASUM 24)
April 28, 2023
Co-opted Council MemberSaqar Altai
May 5, 2023Felix Bende1-3, Bogdan Miutescu1-3, Roxana Șirli1-3
1- Department of Internal Medicine II – Gastroenterology and Hepatology, Center of Advanced Research in Gastroenterology and Hepatology, “Victor Babeș” University of Medicine and Pharmacy Timișoara, Romania
2- Advanced Hepatology Research Center of the Academy of Medical Sciences Timișoara, Romania
3- Department of Gastroenterology, “Pius Brînzeu” County Emergency Hospital, Timișoara, Romania
Clinical history
A 68-year-old male patient, previously diagnosed with stage IV bronchopulmonary cancer (bone metastases and left adrenal gland metastasis) who underwent multiple sessions of chemotherapy and radiotherapy was admitted to the hospital due to abdominal pain, fever, and jaundice. The pain was mostly in the epigastrium and right hypochondrium, while the laboratory tests revealed elevated aminotransferases (2 x normal range), total bilirubin 4 mg/dl, cholestasis (1.5-2 x normal range), leukocytosis, and elevated CRP.
Images
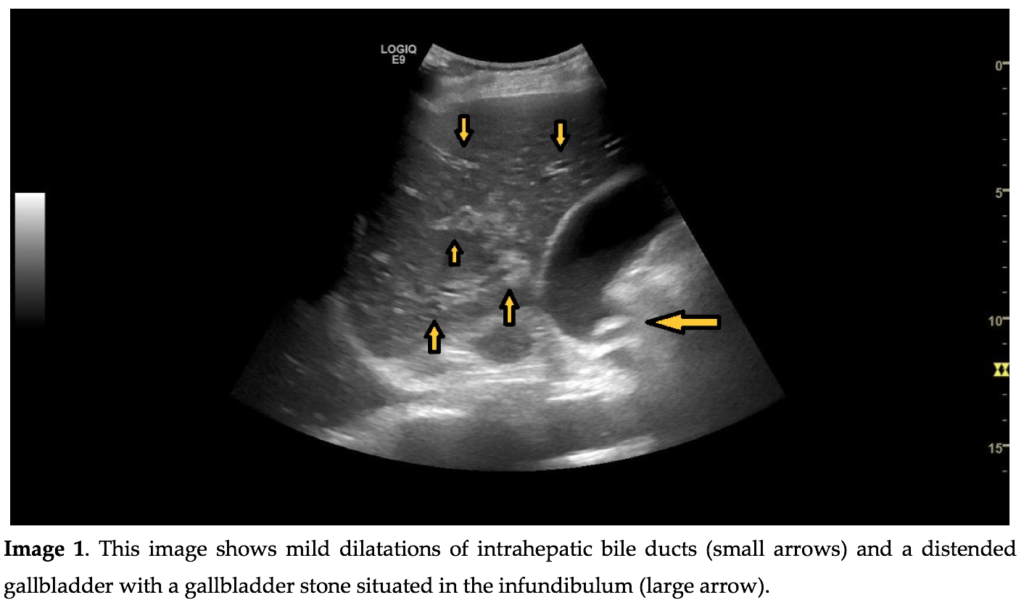
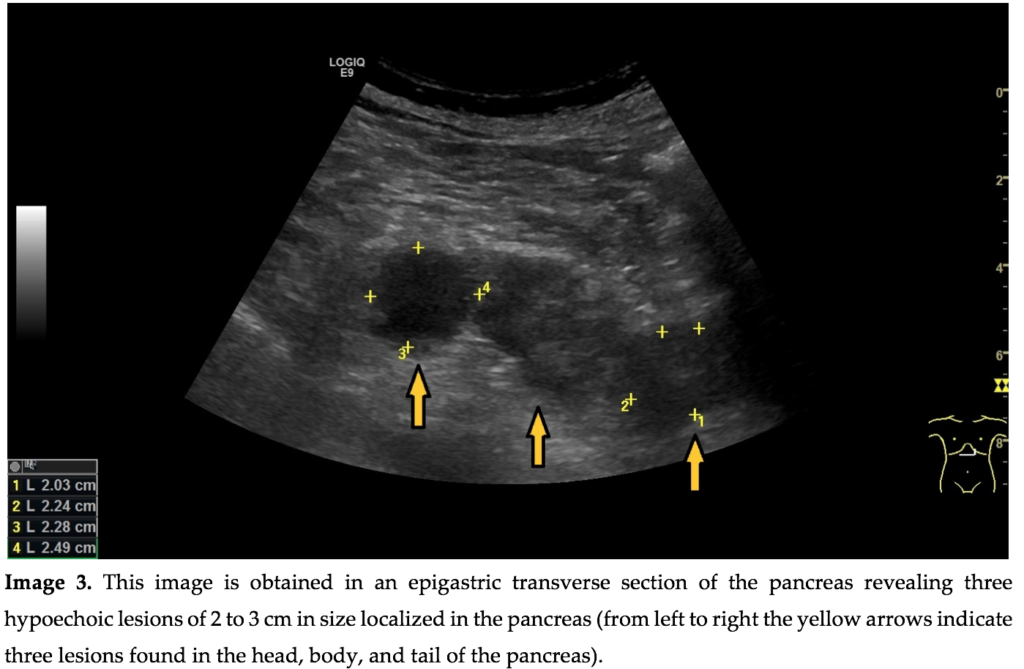
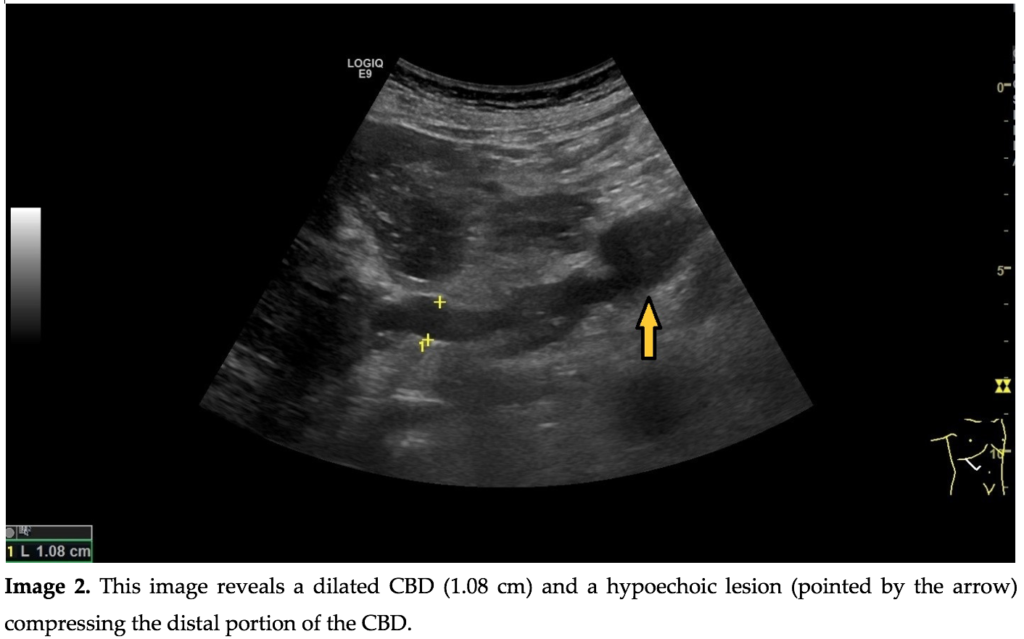
An abdominal US examination revealed dilated intrahepatic bile ducts, a dilated common bile duct (CBD) of approximately 1.1 cm and a distended gallbladder with cholelithiasis. The examination of the pancreas revealed 3 slightly hypoechoic masses of 2 to 3 cm in size situated in the head, body and tail of the pancreas.
Quiz-summary
0 of 2 questions completed
Questions:
- 1
- 2
Information
View the May Case below, answer the question and then click check >
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading...
You must sign in or sign up to start the quiz.
You have to finish following quiz, to start this quiz:
Results
0 of 2 questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 points, (0)
Categories
- Not categorized 0%
- 1
- 2
- Answered
- Review
-
Question 1 of 2
1. Question
Question 1: What is the most likely etiology of the biliary obstruction?
Correct
CORRECT ANSWER EXPLAINED BELOW Correct answer to Q1 is: Pancreatic metastases
Incorrect
CORRECT ANSWER EXPLAINED BELOW Correct answer to Q1 is: Pancreatic metastases
-
Question 2 of 2
2. Question
Discussion
In a patient with jaundice, abdominal US is the first line imaging method recommended for differentiating between obstructive and non-obstructive jaundice. In the presence of signs of obstruction (dilated intrahepatic bile ducts, dilated CBD) abdominal US is very useful for establishing the site and etiology of the obstruction [1].
CBD stones are the most common cause of obstructive jaundice. In the presence of gallbladder stones, CBD stones may be suspected as the cause of the obstruction. They will appear as hyperechoic lesions situated in the CBD lumen, which most frequently generate an “acoustic shadow”. The stone(s) cannot always be visualized by ultrasound, due to the presence of digestive air that prevents an adequate examination of the CBD or because the stone is positioned in the papilla, which makes visualization extremely difficult due to the contact with the gas-filled duodenum.
Pancreatic head adenocarcinoma is another cause of obstructive jaundice. Clinical signs include a progressive painless jaundice, usually accompanied by weight loss. On B-mode US a pancreatic adenocarcinoma appears as a solitary tumor situated in the head of the pancreas that may compress/invade the CBD.
In a patient with obstructive jaundice and a history of any advanced neoplasia, obstruction caused by enlarged lymph nodes in the hepatic hilum should always be suspected. On B-mode US they appear as round hypoechoic masses of variable sizes (2-5 cm).
Pancreatic metastases are rare but should be suspected in a patient with a current or recent history of cancer, especially when multiple solid pancreatic masses are found.
Question 2: What is the next step in the management of this patient?
Correct
CORRECT ANSWER EXPLAINED BELOW Correct answer to Q2 is: GI consult for ERCP and further evaluation of the pancreatic masses
Additional images / videos
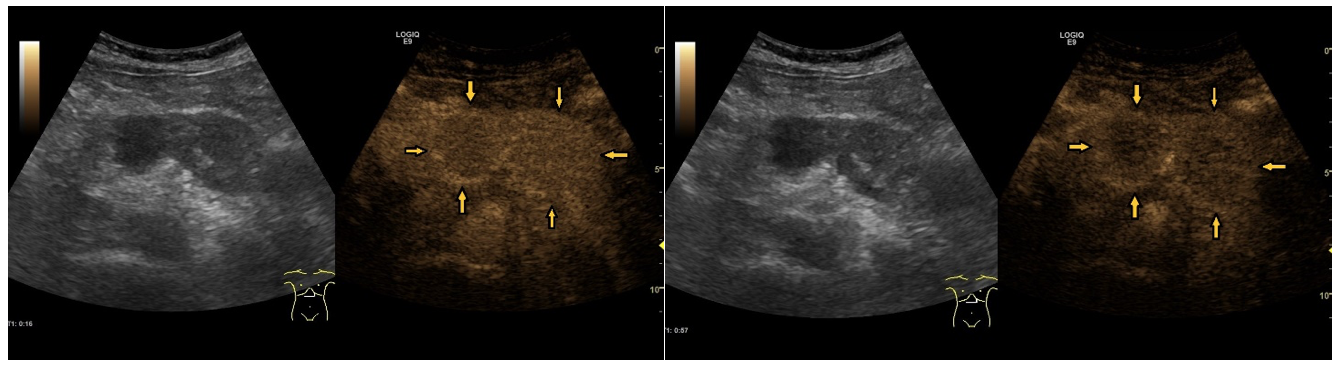
Image 4. CEUS examination of the pancreas shows a rapid enhancement of the pancreatic lesions with a hyper-enhancing rim (left image) followed by subsequent wash-out (right image) indicating the malignant nature of the lesions.
Video 1. – CEUS pancreas. CEUS examination of the pancreas shows a rapid enhancement of the pancreatic lesions with a hyper-enhancing rim, followed by subsequent wash-out, indicating the malignant nature of the lesions.
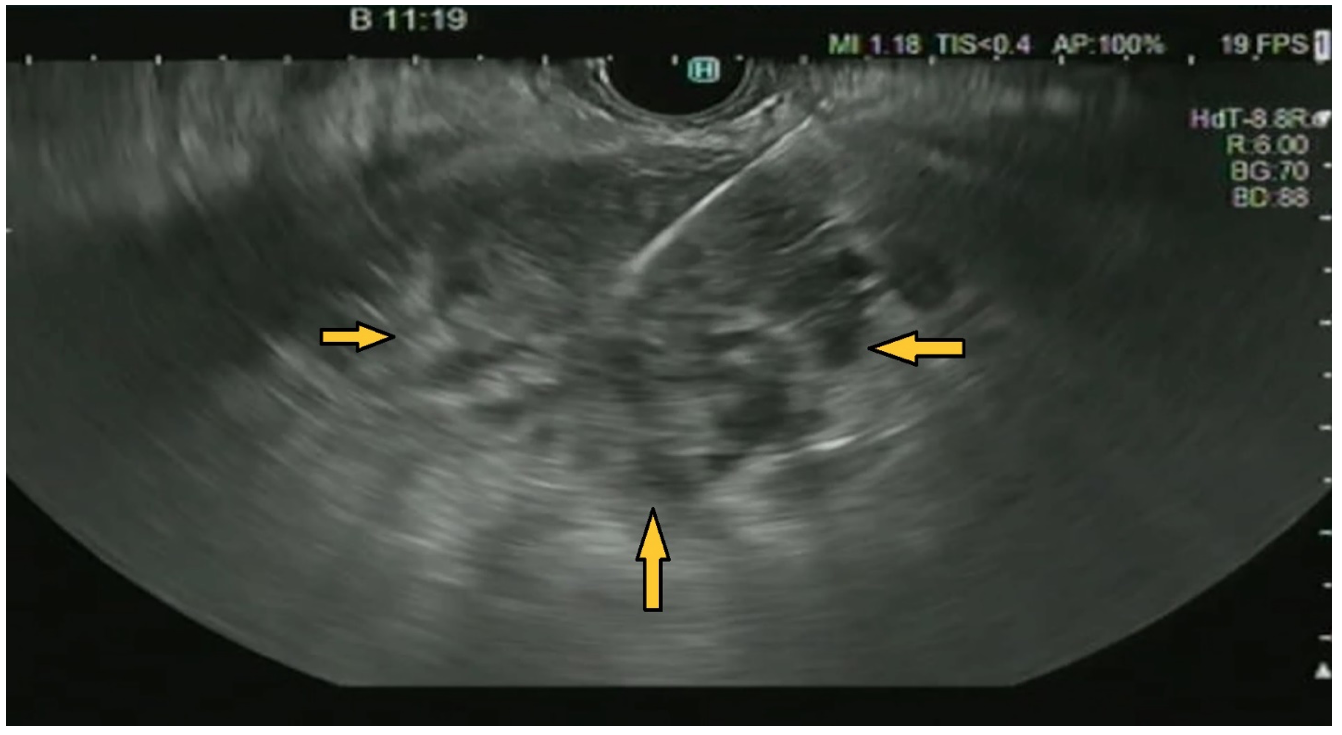
Video 2. – EUS Fine Needle Biopsy (FNB). Endoscopic US FNB from the lesion located in the body of the pancreas. The FNB needle is seen as a linear hyperechoic structure moving inside the hypoechoic lesion.
Image 5. This is an endoscopic US image of a FNB obtained from the lesion located in the body of the pancreas. The FNB needle is seen as a linear hyperechoic image inside the hypoechoic lesion.
Additional Discussion
The correct answer is ERCP with CBD stenting followed by further evaluation of the pancreatic masses: CEUS of the pancreatic lesions, EUS with FNB for histological assessment of the pancreatic lesions.
Pancreatic CEUS is useful in this case because it can be used as an aid to our diagnosis. The pancreatic lesions were enhancing in the arterial phase with a hyper-enhancing rim, followed by wash-out, which is typical for malignancy. In a setting of a solid pancreatic lesion, CEUS can be useful to differentiate between adenocarcinoma and a neuroendocrine tumor [2]. However, there is a lack of published studies evaluating CEUS in pancreatic metastases. Histological assessment is the gold standard. Tissue samples can be obtained by ultrasound-guided fine-needle biopsy (EUS-FNB) or by ultrasound-guided fine-needle aspiration (EUS-FNA) [3].
In the present case, tissue samples were obtained by EUS FNB from the pancreatic lesions situated in the pancreatic head and body and the histopathological result confirmed our main suspicion that the pancreatic lesions were metastases from the primary bronchopulmonary cancer. Before referring the patient to oncology, a computed tomography (CT) of the thorax and abdomen with iv-contrast was performed to evaluate the overall status of the cancer.
The prevalence of pancreatic metastases is quite low. In studies using EUS FNA for different pancreatic lesions the incidence of metastases varies between 0.7% and 10.7% [4-7]. Since radiological examinations are typically performed at an early stage, the incidence of pancreatic metastases in cancer patients undergoing CT is most likely lower than in post-mortem studies in cancer patients.
Pancreatic metastases are most seen in patients with, renal cell, colon, gastric, pancreatic or breast carcinoma.
Conclusion
The peculiarity of this case is that biliary obstruction and cholangitis were caused in an oncological patient by pancreatic metastases (which are quite rare) due to the CBD compression from the pancreatic head metastasis. The patient subsequently underwent successful CBD stenting, antibiotic therapy and was referred to oncology for further management.
Conflicts of Interest:
The author declares no conflict of interest with respect to this case.
References
- Gameraddin M, Omer S, Salih S, Elsayed SA, Alshaikh A: Sonographic evaluation of obstructive jaundice. Open J Med Imaging 2015; 5: 24–29.
- Sidhu PS, Cantisani V, Dietrich CF, Gilja OH, Saftoiu A, Bartels E, Bertolotto M, Calliada F, Clevert DA, Cosgrove D, Deganello A, D’Onofrio M, Drudi FM, Freeman S, Harvey C, Jenssen C, Jung EM, Klauser AS, Lassau N, Meloni MF, Leen E, Nicolau C, Nolsoe C, Piscaglia F, Prada F, Prosch H, Radzina M, Savelli L, Weskott HP, Wijkstra H. The EFSUMB Guidelines and Recommendations for the Clinical Practice of Contrast-Enhanced Ultrasound (CEUS) in Non-Hepatic Applications: Update 2017 (Long Version). Ultraschall Med. 2018 Apr;39(2):e2-e44. English. doi: 10.1055/a-0586-1107. Epub 2018 Mar 6. PMID: 29510439.
- Levine I, Trindade AJ. Endoscopic ultrasound fine needle aspiration vs fine needle biopsy for pancreatic masses, subepithelial lesions, and lymph nodes. World J Gastroenterol. 2021 Jul 14;27(26):4194-4207. doi: 10.3748/wjg.v27.i26.4194. PMID: 34326619; PMCID: PMC8311529.
- Mesa H, Stelow EB, Stanley MW, Mallery S, Lai R, Bardales RH. Diagnosis of nonprimary pancreatic neoplasms by endoscopic ultrasound-guided fine-needle aspiration. Diagn Cytopathol. 2004 Nov;31(5):313-8. doi: 10.1002/dc.20142. PMID: 15468134.
- Layfield LJ, Hirschowitz SL, Adler DG. Metastatic disease to the pancreas documented by endoscopic ultrasound guided fine-needle aspiration: a seven-year experience. Diagn Cytopathol. 2012 Mar;40(3):228-33. doi: 10.1002/dc.21564. Epub 2010 Nov 2. PMID: 22334524.
- Fritscher-Ravens A, Sriram PV, Krause C, Atay Z, Jaeckle S, Thonke F, Brand B, Bohnacker S, Soehendra N. Detection of pancreatic metastases by EUS-guided fine-needle aspiration. Gastrointest Endosc. 2001 Jan;53(1):65-70. doi: 10.1067/mge.2001.111771. PMID: 11154491.
- Gilbert CM, Monaco SE, Cooper ST, Khalbuss WE. Endoscopic ultrasound-guided fine-needle aspiration of metastases to the pancreas: A study of 25 cases. Cytojournal. 2011;8:7. doi: 10.4103/1742-6413.79779. Epub 2011 Apr 21. PMID: 21713016; PMCID: PMC3119417.
Incorrect
CORRECT ANSWER EXPLAINED BELOW Correct answer to Q2 is: GI consult for ERCP and further evaluation of the pancreatic masses
Additional images / videos
Image 4. CEUS examination of the pancreas shows a rapid enhancement of the pancreatic lesions with a hyper-enhancing rim (left image) followed by subsequent wash-out (right image) indicating the malignant nature of the lesions.
Video 1. – CEUS pancreas. CEUS examination of the pancreas shows a rapid enhancement of the pancreatic lesions with a hyper-enhancing rim, followed by subsequent wash-out, indicating the malignant nature of the lesions.
Video 2. – EUS Fine Needle Biopsy (FNB). Endoscopic US FNB from the lesion located in the body of the pancreas. The FNB needle is seen as a linear hyperechoic structure moving inside the hypoechoic lesion.
Image 5. This is an endoscopic US image of a FNB obtained from the lesion located in the body of the pancreas. The FNB needle is seen as a linear hyperechoic image inside the hypoechoic lesion.
Additional Discussion
The correct answer is ERCP with CBD stenting followed by further evaluation of the pancreatic masses: CEUS of the pancreatic lesions, EUS with FNB for histological assessment of the pancreatic lesions.
Pancreatic CEUS is useful in this case because it can be used as an aid to our diagnosis. The pancreatic lesions were enhancing in the arterial phase with a hyper-enhancing rim, followed by wash-out, which is typical for malignancy. In a setting of a solid pancreatic lesion, CEUS can be useful to differentiate between adenocarcinoma and a neuroendocrine tumor [2]. However, there is a lack of published studies evaluating CEUS in pancreatic metastases. Histological assessment is the gold standard. Tissue samples can be obtained by ultrasound-guided fine-needle biopsy (EUS-FNB) or by ultrasound-guided fine-needle aspiration (EUS-FNA) [3].
In the present case, tissue samples were obtained by EUS FNB from the pancreatic lesions situated in the pancreatic head and body and the histopathological result confirmed our main suspicion that the pancreatic lesions were metastases from the primary bronchopulmonary cancer. Before referring the patient to oncology, a computed tomography (CT) of the thorax and abdomen with iv-contrast was performed to evaluate the overall status of the cancer.
The prevalence of pancreatic metastases is quite low. In studies using EUS FNA for different pancreatic lesions the incidence of metastases varies between 0.7% and 10.7% [4-7]. Since radiological examinations are typically performed at an early stage, the incidence of pancreatic metastases in cancer patients undergoing CT is most likely lower than in post-mortem studies in cancer patients.
Pancreatic metastases are most seen in patients with, renal cell, colon, gastric, pancreatic or breast carcinoma.
Conclusion
The peculiarity of this case is that biliary obstruction and cholangitis were caused in an oncological patient by pancreatic metastases (which are quite rare) due to the CBD compression from the pancreatic head metastasis. The patient subsequently underwent successful CBD stenting, antibiotic therapy and was referred to oncology for further management.
Conflicts of Interest:
The author declares no conflict of interest with respect to this case.
References
- Gameraddin M, Omer S, Salih S, Elsayed SA, Alshaikh A: Sonographic evaluation of obstructive jaundice. Open J Med Imaging 2015; 5: 24–29.
- Sidhu PS, Cantisani V, Dietrich CF, Gilja OH, Saftoiu A, Bartels E, Bertolotto M, Calliada F, Clevert DA, Cosgrove D, Deganello A, D’Onofrio M, Drudi FM, Freeman S, Harvey C, Jenssen C, Jung EM, Klauser AS, Lassau N, Meloni MF, Leen E, Nicolau C, Nolsoe C, Piscaglia F, Prada F, Prosch H, Radzina M, Savelli L, Weskott HP, Wijkstra H. The EFSUMB Guidelines and Recommendations for the Clinical Practice of Contrast-Enhanced Ultrasound (CEUS) in Non-Hepatic Applications: Update 2017 (Long Version). Ultraschall Med. 2018 Apr;39(2):e2-e44. English. doi: 10.1055/a-0586-1107. Epub 2018 Mar 6. PMID: 29510439.
- Levine I, Trindade AJ. Endoscopic ultrasound fine needle aspiration vs fine needle biopsy for pancreatic masses, subepithelial lesions, and lymph nodes. World J Gastroenterol. 2021 Jul 14;27(26):4194-4207. doi: 10.3748/wjg.v27.i26.4194. PMID: 34326619; PMCID: PMC8311529.
- Mesa H, Stelow EB, Stanley MW, Mallery S, Lai R, Bardales RH. Diagnosis of nonprimary pancreatic neoplasms by endoscopic ultrasound-guided fine-needle aspiration. Diagn Cytopathol. 2004 Nov;31(5):313-8. doi: 10.1002/dc.20142. PMID: 15468134.
- Layfield LJ, Hirschowitz SL, Adler DG. Metastatic disease to the pancreas documented by endoscopic ultrasound guided fine-needle aspiration: a seven-year experience. Diagn Cytopathol. 2012 Mar;40(3):228-33. doi: 10.1002/dc.21564. Epub 2010 Nov 2. PMID: 22334524.
- Fritscher-Ravens A, Sriram PV, Krause C, Atay Z, Jaeckle S, Thonke F, Brand B, Bohnacker S, Soehendra N. Detection of pancreatic metastases by EUS-guided fine-needle aspiration. Gastrointest Endosc. 2001 Jan;53(1):65-70. doi: 10.1067/mge.2001.111771. PMID: 11154491.
- Gilbert CM, Monaco SE, Cooper ST, Khalbuss WE. Endoscopic ultrasound-guided fine-needle aspiration of metastases to the pancreas: A study of 25 cases. Cytojournal. 2011;8:7. doi: 10.4103/1742-6413.79779. Epub 2011 Apr 21. PMID: 21713016; PMCID: PMC3119417.