Case of the Month July 2021- Palpable inguinal lymph nodes
July 2, 2021WFUMB / EFSUMB Students Webinar Series: 02 September 2021
September 6, 2021Codruta Constantinescu1, Dana Nedelcu2, Nona Bejinariu3, Georgia Baltog2, Alina Constantin2, Cătălin Copăescu2, Adrian Săftoiu1,2
1. Research Center of Gastroenterology and Hepatology Craiova
2. Ponderas Academic Hospital Bucharest
3. Santomar Cluj
* Correspondence: adriansaftoiu@gmail.com / constantinescu.codruta@yahoo.com
Clinical History:
A 32-year-old female with a history of Crohn’s disease for 8 years, receiving intermittent treatment with steroids, immunosuppressants and biologic treatment, had a pericolic abscess drained recently percutaneously. She presented to the Gastroenterology Clinic of Ponderas Academic Hospital, Bucharest, Romania for a second opinion. She had no complaints, no diarrhea and even reported weight gain.
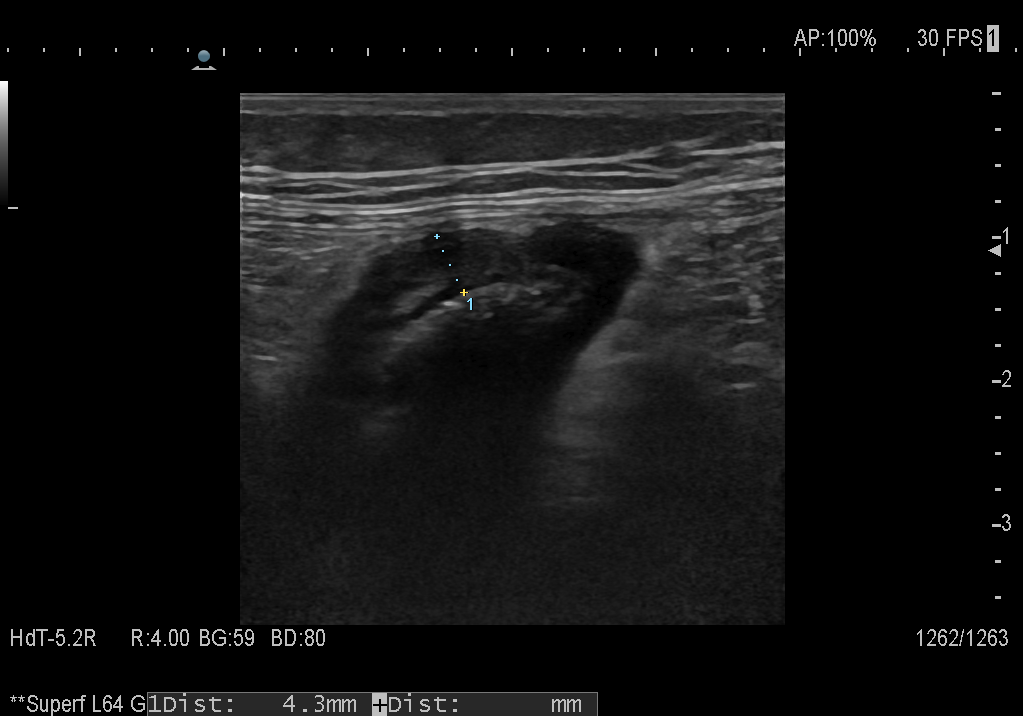
Video: Power Doppler ultrasound shows a hypervascularized bowel wall.
Quiz-summary
0 of 1 questions completed
Questions:
- 1
Information
View the May Case below, answer the question and then click check >
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading...
You must sign in or sign up to start the quiz.
You have to finish following quiz, to start this quiz:
Results
0 of 1 questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 points, (0)
Categories
- Not categorized 0%
- 1
- Answered
- Review
-
Question 1 of 1
1. Question
Question: What is the most likely diagnosis based on the ultrasound findings?
Correct
CORRECT ANSWER EXPLAINED BELOW Correct answer is: Colonic Crohn’s disease
Image findings
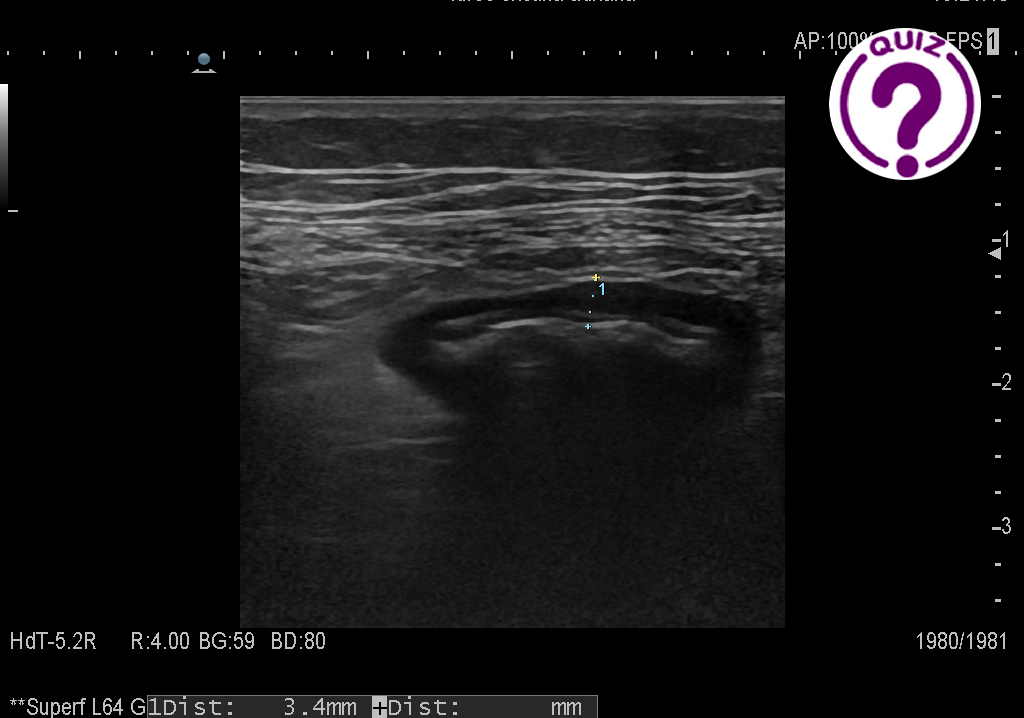
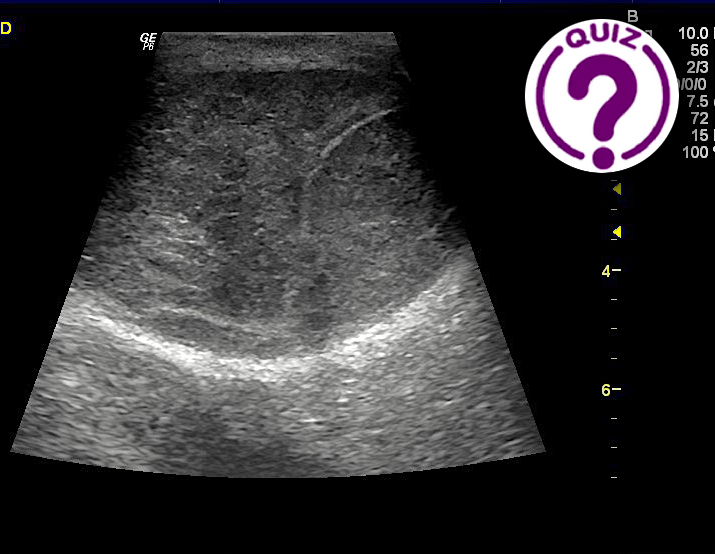
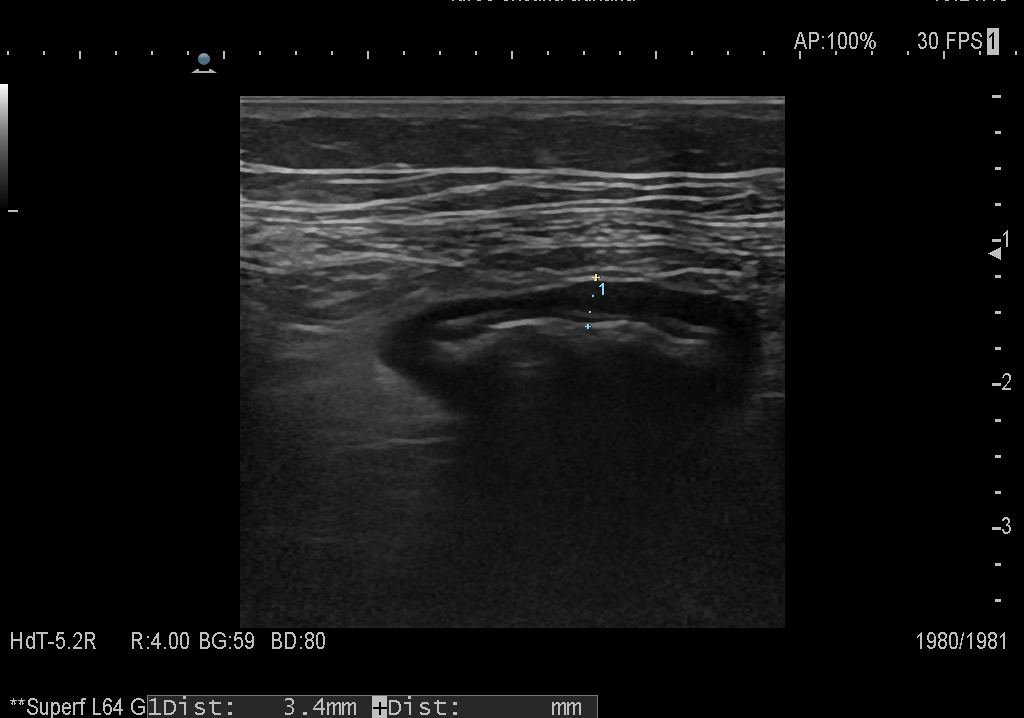
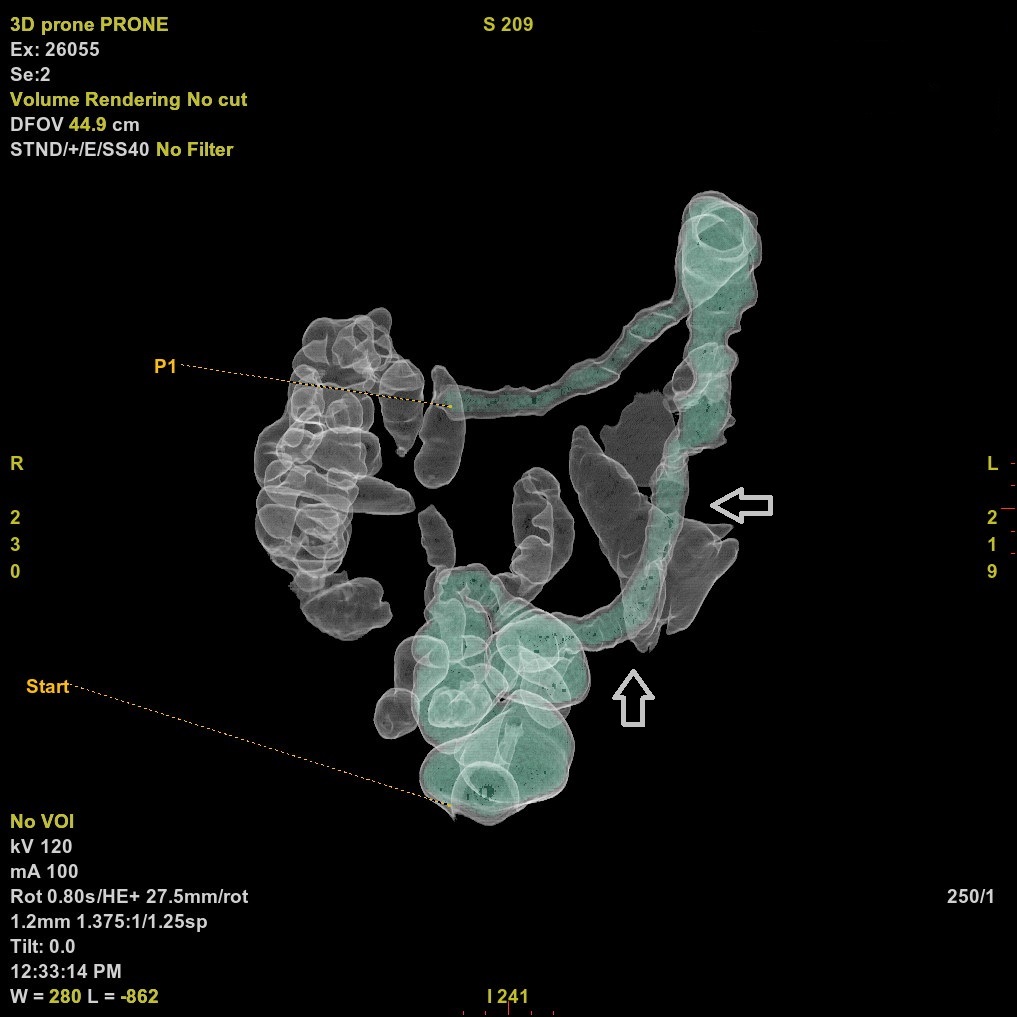
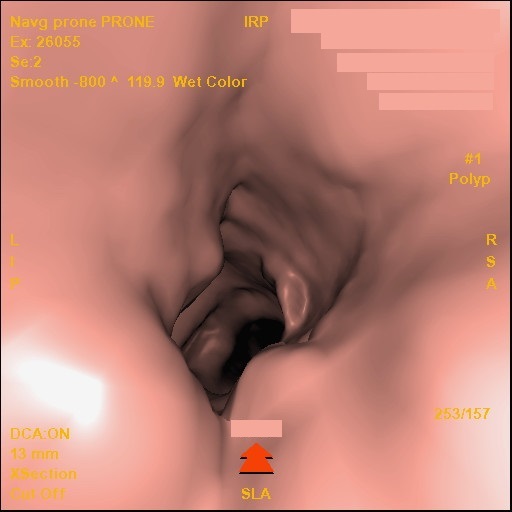
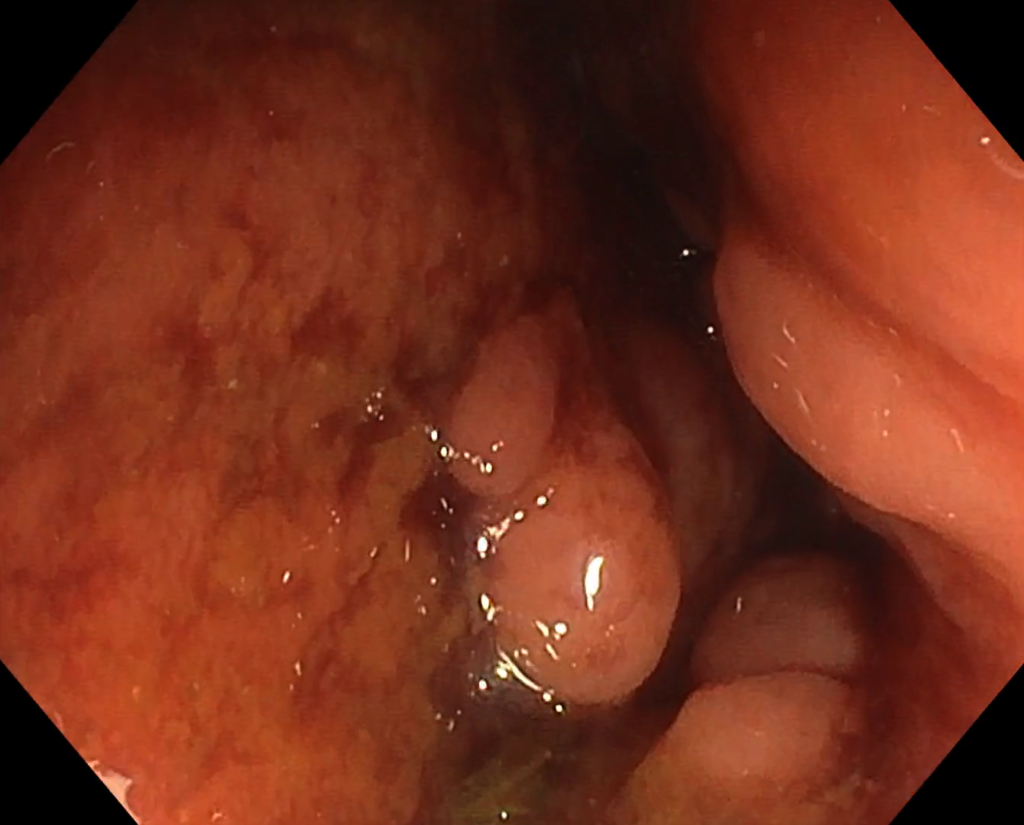
B-mode ultrasound revealed a thickened intestinal wall up to 4-5 mm with luminal narrowing while the stratified appearance of the bowel was lost. CEUS depicts enhancement of all layers in both the arterial as well as the venous phase of contrast-enhancement. Also, Color Doppler showed increased vascularization throughout the affected thickened segment. Furthermore, colonoscopy and CT colonography were performed, revealing the stenosis of the descending colon of about 13 cm long. The virtual colonoscopy also revealed a retroperitoneal fistula located at the level of the descending colon.
Discussion
Patients with Crohn’s disease frequently develop small bowel stricture, while only 15-25% of the patients develop colonic strictures alone (1). It is also known that within 10 years, around 15% of the patients develop a fibrostenotic disease phenotype (2). Usually, patients with stenotic Crohn’s disease may present obstructive symptoms, weight loss, chronic diarrhea or constipation whilst only a small percentage are asymptomatic (3).
Bowel strictures may contain different degrees of inflammation and fibrosis, with a large proportion of patients presenting an overlap between the 2 processes (4). The type of stricture is mostly important for the therapeutic management: inflammatory strictures could benefit from medical treatment, while fibrotic strictures necessitate endoscopic or surgical treatment. In this case, the fact that the colon is still well vascularized would imply that the patient has an inflammatory stricture and might benefit from anti-inflammatory treatment (5). Moreover, ahead of any surgical intervention, this patient was considered eligible to receive a monoclonal antibody drug (vedolizumab).
Regarding the imaging diagnosis, the ultrasound features cannot determine the final etiology of the stenosis. Wall thickening may be caused by several diseases, but as the patient has a history of Crohn’s disease, this is most likely the cause.
Conflicts of Interest
The authors declare no conflict of interest
References
- Freeman HJ. Natural history and clinical behavior of Crohn’s disease extending beyond two decades. J ClinGastroenterol. 2003; 37: 216-219.
- 1 Thia KT, Sandborn WJ, Harmsen WS, et al. Risk factors associated with progression to intestinal complications of Crohn’s disease in a population-based cohort. Gastroenterology. 2010; 139: 1147-1155.
- Bettenworth D, Bokemeyer A, Baker M, et al. Assessment of Crohn’s disease-associated small bowel strictures and fibrosis on cross-sectional imaging: a systematic review. Gut. 2019; 68: 1115-1126.
- Maconi G, Nylund K, Ripolles T, Calabrese E, Dirks K, Dietrich CF, Hollerweger A, Sporea I, Saftoiu A, Maaser C, Hausken T, Higginson AP, Nürnberg D, Pallotta N, Romanini L, Serra C, Gilja OH.EFSUMB Recommendations and Clinical Guidelines for Intestinal Ultrasound (GIUS) in Inflammatory Bowel Diseases.Ultraschall Med. 2018;39:304-317.
- Ripollés T, Rausell N, Paredes JM, Grau E, Martínez MJ, Vizuete J.Effectiveness of contrast-enhanced ultrasound for characterisation of intestinal inflammation in Crohn’s disease: a comparison with surgical histopathology analysis.J Crohns Colitis. 2013;7:120-8.
Incorrect
CORRECT ANSWER EXPLAINED BELOW Correct answer is: Colonic Crohn’s disease
Image findings
B-mode ultrasound revealed a thickened intestinal wall up to 4-5 mm with luminal narrowing while the stratified appearance of the bowel was lost. CEUS depicts enhancement of all layers in both the arterial as well as the venous phase of contrast-enhancement. Also, Color Doppler showed increased vascularization throughout the affected thickened segment. Furthermore, colonoscopy and CT colonography were performed, revealing the stenosis of the descending colon of about 13 cm long. The virtual colonoscopy also revealed a retroperitoneal fistula located at the level of the descending colon.
Discussion
Patients with Crohn’s disease frequently develop small bowel stricture, while only 15-25% of the patients develop colonic strictures alone (1). It is also known that within 10 years, around 15% of the patients develop a fibrostenotic disease phenotype (2). Usually, patients with stenotic Crohn’s disease may present obstructive symptoms, weight loss, chronic diarrhea or constipation whilst only a small percentage are asymptomatic (3).
Bowel strictures may contain different degrees of inflammation and fibrosis, with a large proportion of patients presenting an overlap between the 2 processes (4). The type of stricture is mostly important for the therapeutic management: inflammatory strictures could benefit from medical treatment, while fibrotic strictures necessitate endoscopic or surgical treatment. In this case, the fact that the colon is still well vascularized would imply that the patient has an inflammatory stricture and might benefit from anti-inflammatory treatment (5). Moreover, ahead of any surgical intervention, this patient was considered eligible to receive a monoclonal antibody drug (vedolizumab).
Regarding the imaging diagnosis, the ultrasound features cannot determine the final etiology of the stenosis. Wall thickening may be caused by several diseases, but as the patient has a history of Crohn’s disease, this is most likely the cause.
Conflicts of Interest
The authors declare no conflict of interest
References
- Freeman HJ. Natural history and clinical behavior of Crohn’s disease extending beyond two decades. J ClinGastroenterol. 2003; 37: 216-219.
- 1 Thia KT, Sandborn WJ, Harmsen WS, et al. Risk factors associated with progression to intestinal complications of Crohn’s disease in a population-based cohort. Gastroenterology. 2010; 139: 1147-1155.
- Bettenworth D, Bokemeyer A, Baker M, et al. Assessment of Crohn’s disease-associated small bowel strictures and fibrosis on cross-sectional imaging: a systematic review. Gut. 2019; 68: 1115-1126.
- Maconi G, Nylund K, Ripolles T, Calabrese E, Dirks K, Dietrich CF, Hollerweger A, Sporea I, Saftoiu A, Maaser C, Hausken T, Higginson AP, Nürnberg D, Pallotta N, Romanini L, Serra C, Gilja OH.EFSUMB Recommendations and Clinical Guidelines for Intestinal Ultrasound (GIUS) in Inflammatory Bowel Diseases.Ultraschall Med. 2018;39:304-317.
- Ripollés T, Rausell N, Paredes JM, Grau E, Martínez MJ, Vizuete J.Effectiveness of contrast-enhanced ultrasound for characterisation of intestinal inflammation in Crohn’s disease: a comparison with surgical histopathology analysis.J Crohns Colitis. 2013;7:120-8.