Uncategorized
- All
- 25th May Pre Congress
- 26th May Day 1 Congress
- 28th May Day 3 Congress
- Administrative Councillors
- books
- Chairs
- Clinical Ultrasound
- COE Centre
- COE Task Force
- Collaboration Committee
- Committees
- Congress 2022
- Congress Committee
- Congress News
- Constitution Committee
- E-Book
- E-learning Task Force
- echoes
- Education Committee
- EXB
- Featured
- Featured_Congresses
- Featured_External Meetings
- Featured_Federation
- In Memoriam
- Investment Advisory Committee
- NEWS
- NEWS CoE's
- NEWS Partnerships
- Nominating Committee
- Pioneers
- Publications Committee
- Room 1 - Alfa 1
- Room 1 - Alfa 1
- Room 2 - Alfa 2
- Room 2 - Alfa 2
- Room 3 - Alfa 3
- Room 4 - Atena
- Room 4 - Atena
- Room 5 - Viena
- Room 6 - Roma 1
- Room 7 - Roma 2
- Room 8- Oslo
- Safety Committee
- Safety Statements
- Student Education
- Ultrasound the Best
- UMB Publications
- Uncategorized
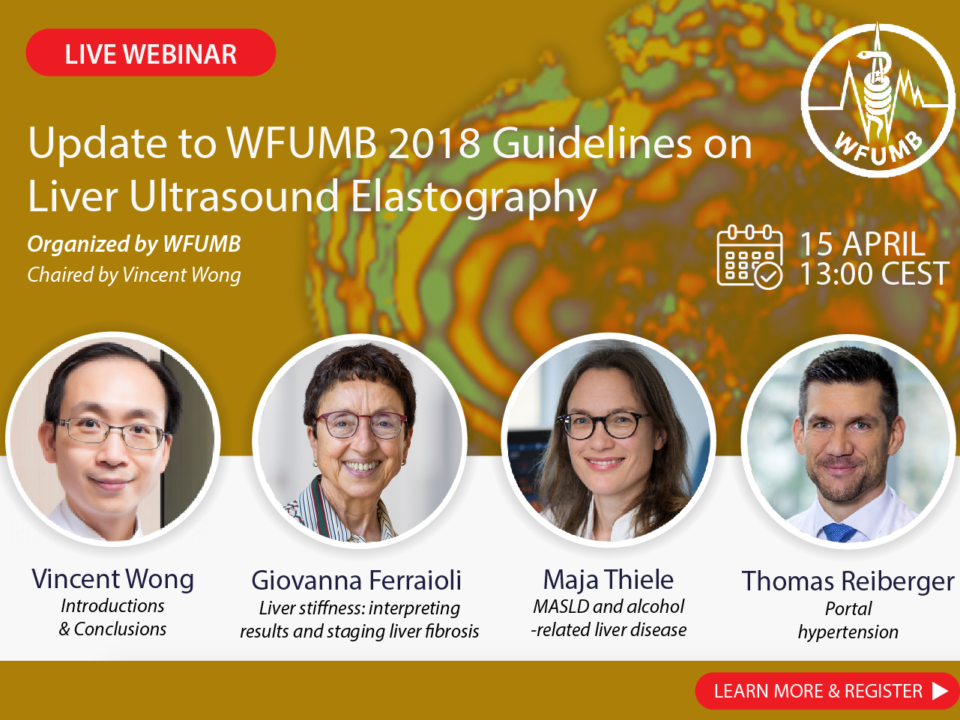
- Webinars
- WIOTM
May 8, 2024
April 19, 2024
April 19, 2024